Post-Inflammatory Erythema: Causes, Treatment, and Tips

Post-Inflammatory Erythema (PIE) is a common skin concern that appears after inflammation, such as acne, has subsided.[1WebMD: What to Know About Post-Inflammatory Erythema.] Even when the pimple is gone, the affected area may still look red or pink. Medically, PIE is caused by the dilation and increased number of capillaries near the skin’s surface due to inflammation. This results in more blood flow to the area, creating a reddish mark that lingers.
Unlike hyperpigmentation, which is caused by excess melanin, PIE is vascular in nature—making the marks appear red, pink, or even purplish, especially on fair skin. According to dermatologist Dr. Marisa Garshick, acne inflammation triggers a vascular response that can keep the skin looking irritated long after the breakout has healed.
PIE can last for weeks or even months, depending on your skin type and how severe the inflammation was. Understanding what causes PIE and how to treat it effectively is the first step to restoring an even-toned, healthy complexion. Let’s explore expert-approved solutions and tips to fade these red marks safely.
What Is Post-Inflammatory Erythema?
Post-Inflammatory Erythema (PIE) refers to the red or pink marks left behind after inflamed skin—especially acne—has healed.[2Healthline: How to Treat Post-Inflammatory Erythema.] It typically occurs after inflammatory breakouts, such as papules (small red bumps) or pustules (pus-filled pimples), not from non-inflammatory types like blackheads or whiteheads.
Dr. Farhaad Riyaz explains that PIE develops due to damaged or dilated blood vessels in the skin. The discoloration can vary, ranging from light pink to deep red, depending on the severity of inflammation and your skin’s healing process. While it’s most common on the face, PIE can also appear on the neck, chest, or back—areas frequently affected by acne.
People with fair skin are more prone to PIE, while those with darker skin tones often develop Post-Inflammatory Hyperpigmentation (PIH), which leaves behind dark brown or grayish spots due to excess melanin. Knowing the difference between PIE and PIH is essential for choosing the right skincare products and treatments.
What Causes Post-Inflammatory Erythema?
1. Excess Oil Production
According to Dr. Farhaad Riyaz, acne-prone skin typically produces more sebum (oil) than normal skin. Not only is the amount excessive, but the texture is also thicker and stickier—making it more likely to clog pores and cause breakouts.
On a biochemical level, acne-prone skin often lacks essential fatty acids like linoleic acid, which helps support the skin barrier and regulate inflammation.[3charlotte rye: The Gut-Skin Axis: How Nutrition Supports a Healthy Skin Barrier.] At the same time, levels of squalene and wax esters—other components of sebum—tend to be elevated. This imbalance creates a favorable environment for acne-causing bacteria such as Cutibacterium acnes to thrive.
Understanding this oil composition is crucial for choosing effective treatments. Skincare products that regulate sebum production while restoring lipid balance can help reduce inflammation and prevent PIE from forming in the first place.
2. Acne-Causing Bacteria
The skin naturally hosts bacteria, including Cutibacterium acnes (formerly Propionibacterium acnes). However, people with acne often have higher concentrations of this bacteria. It thrives in clogged pores, feeding on trapped oil.
Dr. Riyaz explains that as C. acnes digests the excess oil, it releases irritating byproducts, including free fatty acids. These substances trigger an immune response that leads to inflammation, redness, and pimple formation. Even after the active acne clears, the residual redness—caused by dilated blood vessels—remains as PIE.
PIE is not an active infection but a lingering vascular response. Controlling bacterial growth with targeted skincare—such as topical antibacterials like benzoyl peroxide or clindamycin—can reduce inflammation and lower the risk of developing PIE.[4MID County Dermatology: Effective Acne Treatment Options in St. Louis: Benzoyl Peroxide.]
3. How Harsh Skincare Products Can Worsen Post-Inflammatory Erythema
Using harsh or unsuitable skincare products can trigger or worsen Post-Inflammatory Erythema (PIE).[5Natural Image Skincenter: Post-Inflammatory Erythema vs. Post-Inflammatory Hyperpigmentation.] According to Dr. Marisa Garshick, although active ingredients like retinoids, salicylic acid, and benzoyl peroxide are effective against acne, overusing them—or combining too many at once—can damage the skin barrier. This leads to irritation, redness, and inflammation, increasing the chances of PIE developing.
Products such as strong cleansers with sulfates, gritty facial scrubs, or alcohol-based toners can strip the skin of its natural oils and disrupt the barrier. A weakened barrier leaves skin more sensitive to irritants and prone to inflammation—especially if the skin is already healing from acne.[6L’Occitane: Damaged Skin Barrier Characteristics, Causes, & Solutions.]
To avoid triggering PIE, it’s important to choose gentle, non-comedogenic products that match your skin type. Avoid layering too many actives at once, and prioritize soothing and barrier-repairing ingredients to keep your skin balanced and less reactive.
4. How Popping Pimples Can Lead to PIE
Picking, squeezing, or scratching acne can significantly increase your risk of developing Post-Inflammatory Erythema (PIE).[7Kins Clinic: Post Inflammatory Erythema from Acne: A Guide to Causes and Treatments.] Dr. Marisa Garshick explains that this habit damages the surrounding skin tissue and deepens inflammation, often leaving long-lasting red or pink marks after the acne heals. In some cases, it may also lead to permanent scarring or secondary infection.
When you pop a pimple, it creates trauma that causes the blood vessels underneath to dilate, leading to PIE. This mechanical pressure extends the inflammation process, making redness worse and more persistent.
If you’ve already popped a pimple and it scabs over, treat it like a wound: keep the area clean, don’t pick at the scab, and apply healing ointments to support skin repair. For large or inflamed breakouts, Dr. Garshick recommends considering a cortisone injection from a dermatologist. This treatment can reduce swelling quickly, calm inflammation, and lower the chances of both PIE and scarring.
5. The Role of Hormones in Acne and PIE
Hormonal changes are a major trigger for acne—and indirectly, Post-Inflammatory Erythema (PIE). According to Dr. Farhaad Riyaz, rising androgen levels like testosterone can increase oil production in the sebaceous glands. When excess oil mixes with dead skin cells and bacteria, clogged pores and inflammatory acne follow.
Hormonal fluctuations can happen during puberty, menstruation, PCOS, perimenopause, or menopause. In women, hormonal breakouts often appear on the chin and jawline, especially before their period.
Hormonal acne tends to be deeper and more inflamed, which raises the risk of PIE after healing. Understanding the hormonal aspect of acne is essential for effective treatment—whether through topical products, oral contraceptives, hormone therapy, or guidance from a dermatologist or endocrinologist. Managing hormonal breakouts properly helps prevent PIE from forming later.
6. Dead Skin Cell Buildup and Its Link to Acne and PIE
One often-overlooked cause of acne—and PIE—is the buildup of dead skin cells. Dr. Farhaad Riyaz notes that acne-prone skin produces more dead skin cells, and these don’t shed properly due to disrupted cell turnover. In fact, studies show acne-prone individuals can produce up to five times more dead skin cells than normal skin.
What makes it worse is that these cells are also stickier, making them harder to shed naturally. This condition, known as retention hyperkeratosis, causes clogged pores and triggers inflammation when mixed with excess oil and bacteria.
If the breakout becomes severe, the resulting inflammation can leave behind PIE—red or pink spots that linger after acne has cleared. Regular gentle exfoliation with ingredients like salicylic acid or natural enzymes can help remove buildup and prevent clogged pores, without compromising the skin barrier or causing irritation.
How Long Does Post-Inflammatory Erythema Last?
Post-Inflammatory Erythema (PIE) can last anywhere from a few weeks to several months, depending on the severity of inflammation, your skin type, and how you care for your skin. While PIE typically fades over time on its own, using the right skincare can help speed up the healing process.
Gentle, anti-inflammatory ingredients—such as niacinamide, azelaic acid, or centella asiatica—can calm redness and support recovery. Consistent use of sunscreen is also key, as UV exposure can worsen discoloration and slow down healing. Patience and a gentle routine are your best allies in fading PIE and restoring an even skin tone.
About the Author
M. Hariri is a business and beauty content writer with over five years of experience. He focuses on research-based skincare education and frequently collaborates with dermatologists. His work can be found in various national and international beauty publications.






 Acne
Acne Anti-Aging
Anti-Aging Business
Business Digital Marketing
Digital Marketing Economics
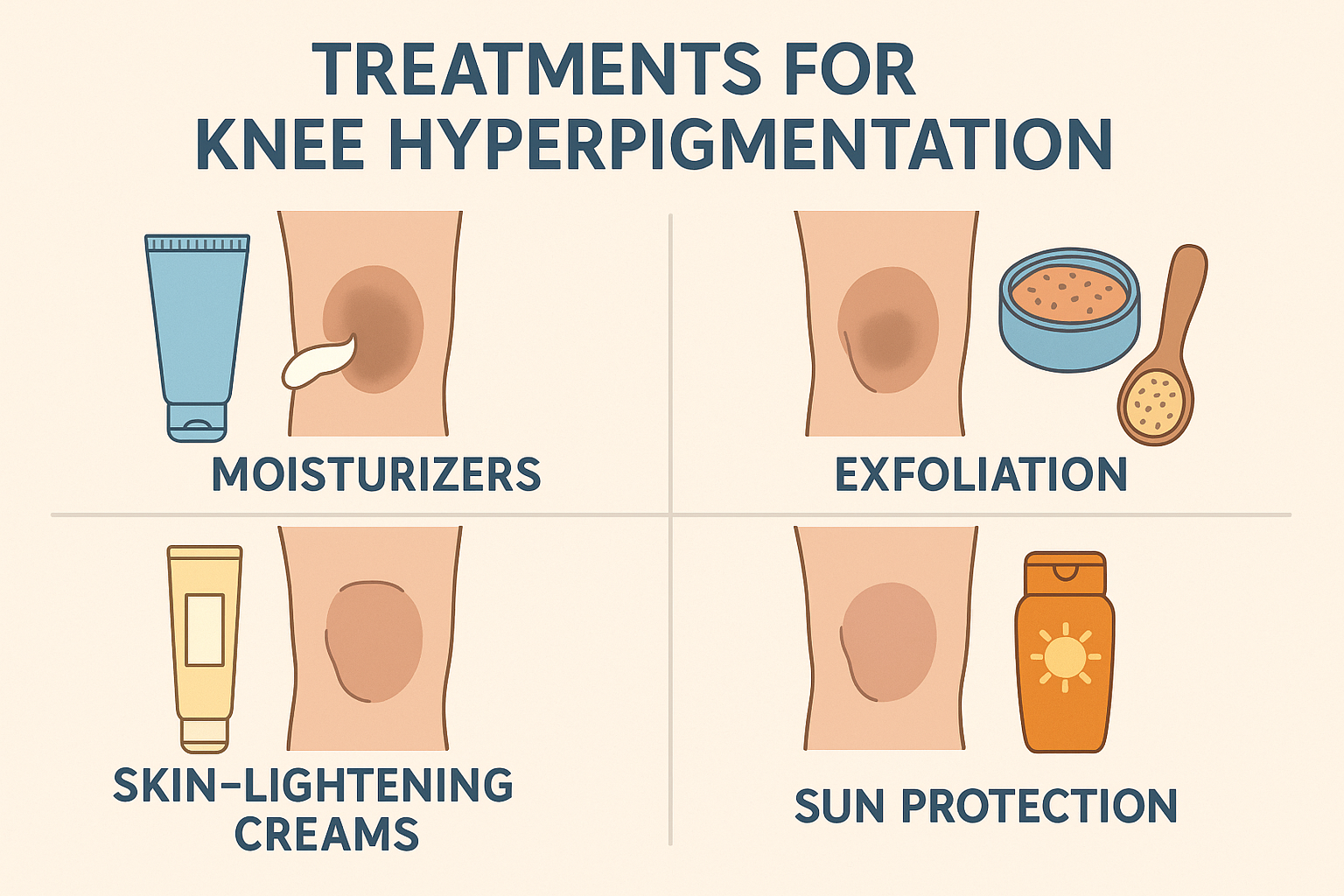
Economics Exfoliation
Exfoliation Hair Removal
Hair Removal Movies
Movies Personal Finance
Personal Finance Websites
Websites