Does Ovulation Cause Acne? Dermatologists Explain Why
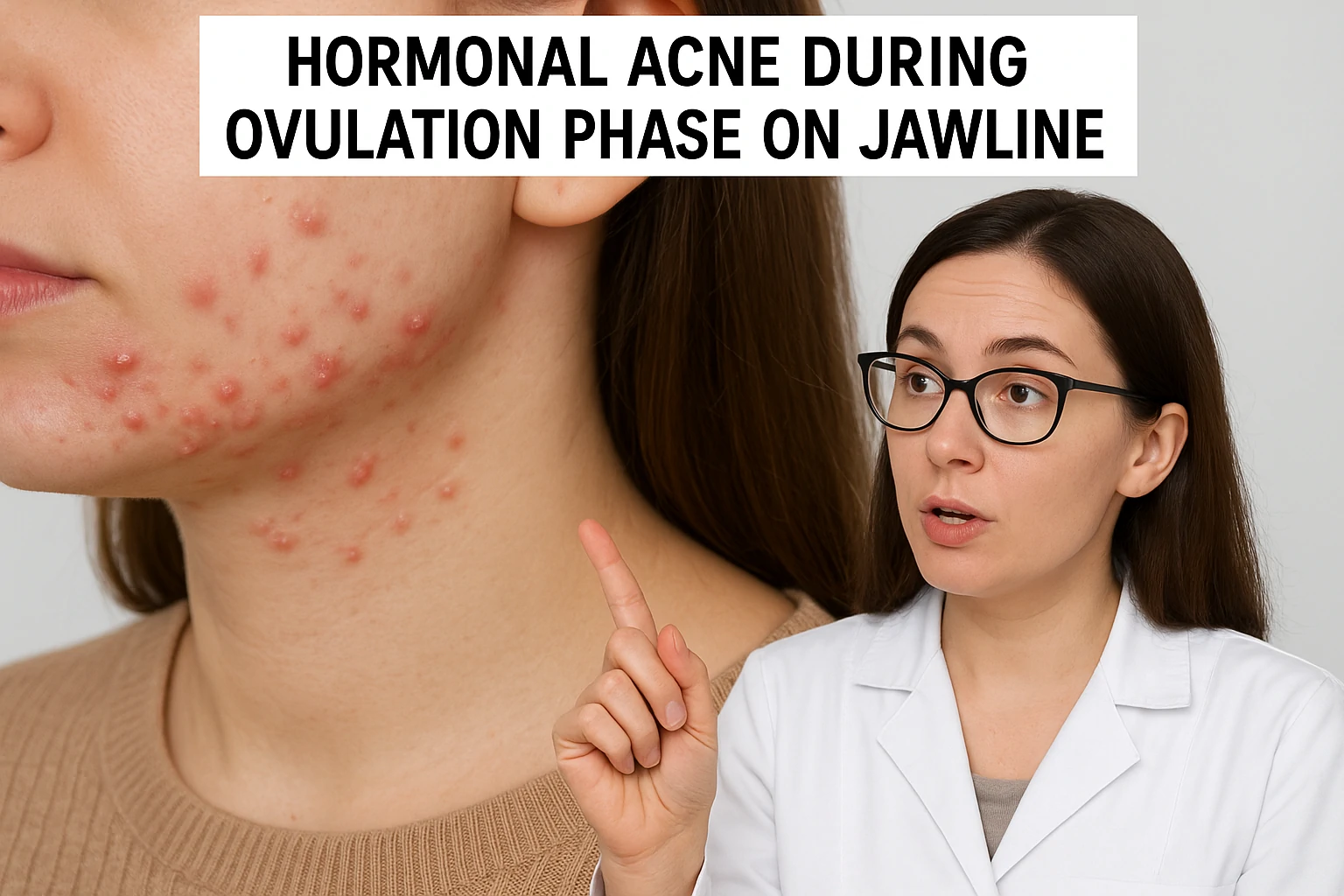
Many women notice that acne often flares up at specific times during their menstrual cycle—especially around ovulation. But what exactly links ovulation to breakouts?
Dermatologists explain that hormonal fluctuations, particularly spikes in progesterone and androgens during ovulation, trigger an increase in oil (sebum) production. This excess oil can clog pores and lead to acne, especially along the chin and jawline.
This type of acne is known as hormonal acne. It tends to follow a predictable pattern and often recurs during certain phases of the menstrual cycle. According to Dr. Morgan Rabach, a board-certified dermatologist, understanding your skin’s hormonal timeline is the first step toward better acne management.
If you’ve noticed monthly breakouts that seem to sync with your cycle, you’re not alone. Keep reading to learn what hormonal acne really is and how to treat it effectively—backed by expert advice.
What Exactly Is Hormonal Acne?
Hormonal acne is caused by internal hormonal shifts rather than external factors like bacteria or clogged pores from makeup. It’s most common in adults, especially women in their 20s to 40s.
Experts say hormonal fluctuations—such as those during menstruation, stress, or hormonal disorders—can stimulate excess sebum production. This oil clogs pores, leading to inflamed, painful pimples that often appear deep under the skin.
This type of acne typically shows up around the lower face—think chin, jaw, and neck. It often comes and goes with your monthly cycle.
Recognizing the signs of hormonal acne helps you choose the right treatment. From skincare that targets oil control and inflammation, to hormonal therapy or prescription retinoids—getting professional advice early can make all the difference.
How Your Period Affects the Skin
Your skin changes daily throughout your menstrual cycle—not just during your period. These changes are driven by natural hormonal shifts.
A typical cycle lasts about 28 days. During the first half, estrogen levels rise. Estrogen improves skin texture, reduces inflammation, and boosts hydration—often giving your skin a healthy, glowing look.
In the second half, progesterone becomes dominant. It increases sebum production, making skin oilier and more prone to clogged pores. At the same time, testosterone levels may rise, further stimulating oil glands.
When progesterone and testosterone peak together, hormonal acne can flare up—especially in the form of deep, red, and persistent breakouts.[1Elsaie ML. Hormonal treatment of acne vulgaris: an update. Clin Cosmet Investig Dermatol. 2016 Sep 2;9:241-8. doi: 10.2147/CCID.S114830.]
Understanding this rhythm can help you adjust your skincare routine throughout the month, maximizing effectiveness and preventing flare-ups.
How to Track Skin Changes During Your Menstrual Cycle
If your breakouts tend to occur at the same point every month, they’re likely hormonal. That’s why tracking your menstrual cycle is key.
Dermatologists recommend keeping a skincare and period diary to spot patterns. For example, if your acne consistently shows up a few days before your period, hormonal shifts are likely the culprit.
Knowing your skin’s “problem weeks” helps you plan targeted treatments in advance—like switching to oil-controlling cleansers or avoiding heavy products when you’re more prone to breakouts.
Being proactive allows for smarter, cycle-aware skincare. Over time, this can help reduce flare-ups and improve skin resilience.
1. Follicular Phase
Though menstruation marks the start of the cycle medically, dermatologists often highlight the follicular phase (about 7–10 days after your period ends) as the skin’s healthiest window.[2Bull JR, Rowland SP, Scherwitzl EB, Scherwitzl R, Danielsson KG, Harper J. Real-world menstrual cycle characteristics of more than 600,000 menstrual cycles. NPJ Digit Med. 2019 Aug 27;2:83. doi: 10.1038/s41746-019-0152-7.]
During this time, estrogen rises steadily. It boosts collagen, elastin, and cell turnover—leading to plumper, more hydrated, and clearer skin. Pores look smaller, and skin tone becomes more even.
Clinically, this is when skin is most balanced—neither too dry nor too oily. It’s the perfect time to reinforce your skincare routine with brightening serums, lightweight moisturizers, and exfoliants to maintain that post-period glow.
If you’re planning to start or reset your skincare regimen, this phase offers the best foundation for visible improvements.
2. Ovulation Phase
The ovulation phase lasts about 3 to 5 days and marks a key hormonal turning point in your menstrual cycle.
During this phase, follicle-stimulating hormone (FSH) rises, followed by a surge in luteinizing hormone (LH), which triggers the release of an egg.[3Raju GA, Chavan R, Deenadayal M, Gunasheela D, Gutgutia R, Haripriya G, Govindarajan M, Patel NH, Patki AS. Luteinizing hormone and follicle stimulating hormone synergy: A review of role in controlled ovarian hyper-stimulation. J Hum Reprod Sci. 2013 Oct;6(4):227-34. doi: 10.4103/0974-1208.126285.] Estrogen remains high, and testosterone levels start to climb. Progesterone also begins to increase as ovulation approaches.[4Bull JR, Rowland SP, Scherwitzl EB, Scherwitzl R, Danielsson KG, Harper J. Real-world menstrual cycle characteristics of more than 600,000 menstrual cycles. NPJ Digit Med. 2019 Aug 27;2:83. doi: 10.1038/s41746-019-0152-7.]
According to dermatologists, these hormone shifts can stimulate oil (sebum) production, making skin feel greasier—especially if you’re sensitive to hormonal changes.
Although your skin may start to feel oilier during ovulation, breakouts usually don’t peak until the next stage: the luteal phase. Recognizing these early changes allows you to adjust your skincare routine ahead of time, helping to prevent clogged pores and inflammation before they start.
3. Luteal Phase
The luteal phase, which lasts about 10 to 14 days, is when hormonal acne often becomes most noticeable.
During this time, estrogen levels drop while progesterone spikes. The ratio of testosterone to estrogen increases, prompting excess sebum production and clogged pores. This hormonal imbalance can trigger painful, inflamed acne—especially around the jawline and cheeks.
Progesterone may also cause skin to appear puffier and oilier. With your body temperature slightly elevated and oil production at its peak, acne-causing bacteria like Cutibacterium acnes thrive, worsening inflammation.
Toward the end of this phase, the rapid drop in estrogen and progesterone can leave skin looking dull and dehydrated. Increased prostaglandins may also heighten skin sensitivity. Experts suggest avoiding harsh treatments like waxing during this time to minimize irritation.
4. Menstrual Phase
The menstrual phase spans 3 to 7 days and is marked by the sharpest drop in reproductive hormones—estrogen, progesterone, and testosterone.
This decline can actually offer some skin relief. As acne-triggering hormones fall, inflammation often begins to subside, and existing breakouts may start to heal.
However, lower estrogen levels can also lead to dryness, sensitivity, and a dull complexion. As a result, your skin may feel tight or flaky, especially toward the end of this phase.
Dermatologists recommend focusing on hydration and barrier repair. Moisturizers with soothing ingredients like hyaluronic acid or ceramides are ideal to restore comfort and protect against environmental stressors.
Understanding this phase helps you care for your skin with a gentler, more supportive approach—setting the stage for a healthier glow in the upcoming follicular phase.
Is Your Acne Hormonal?
Wondering if your breakouts are tied to your hormones? Timing and location are two major clues.
Hormonal acne typically appears during the luteal phase, just before your period.[5Geller L, Rosen J, Frankel A, Goldenberg G. Perimenstrual flare of adult acne. J Clin Aesthet Dermatol. 2014 Aug;7(8):30-4.] It most commonly affects the lower face, including the jawline, chin, cheeks, and sometimes the upper neck. These breakouts can range from deep, painful cysts to whiteheads and blackheads.
If your acne flares up in the same areas at the same time each month, it’s a strong sign hormones are involved. Still, dermatologists caution that acne location alone isn’t enough for a full diagnosis.
If you also experience irregular periods, sudden weight gain, or excess facial hair, it may signal an underlying hormonal imbalance—like PCOS—that requires medical attention.
Consulting a dermatologist can help you confirm the root cause and guide you to the right treatment plan
Best Ways to Treat Hormonal Acne
Dealing with hormonal acne can be frustrating—especially when breakouts return month after month despite trying over-the-counter products.
While hormones can’t be controlled entirely, you can still manage their impact on your skin through strategic care and medical guidance.
Hormonal acne often requires more than just a surface-level approach. If breakouts are severe, persistent, or painful, prescription treatments may be necessary. Dermatologists may recommend topical retinoids, oral medications like spironolactone, or even hormonal therapy, depending on your skin and hormone profile.
Lifestyle also plays a key role. A balanced diet, stress management, and consistent skincare can all support your treatment efforts.
In the next section, we’ll explore evidence-based treatments and daily skincare routines that can help calm hormonal acne and keep your skin in balance.
1. Topical Treatments for Hormonal Acne
Topical medications are often the first step in treating hormonal acne—especially if breakouts are mild to moderate. Dermatologists typically recommend starting here before moving on to oral treatments.
Common topical options include:[6Bagatin E, Freitas THP, Rivitti-Machado MC, Machado MCR, Ribeiro BM, Nunes S, Rocha MADD. Adult female acne: a guide to clinical practice. An Bras Dermatol. 2019 Jan-Feb;94(1):62-75. doi: 10.1590/abd1806-4841.20198203.]
- Tretinoin (Retin-A): A retinoid that speeds up skin cell turnover and helps clear clogged pores.
- Dapsone (Aczone): Originally used for leprosy, this gel has strong anti-inflammatory and antibacterial effects.
- Clindamycin: A topical antibiotic that reduces acne-causing bacteria and inflammation.
While these treatments can be effective, experts note that they don’t target the hormonal root cause. That’s where newer innovations like clascoterone (Winlevi) come in. This topical anti-androgen works by blocking testosterone activity in the skin, reducing oil production and inflammation—making it an exciting breakthrough for hormonal acne.
If over-the-counter options aren’t cutting it, consult a dermatologist for a prescription tailored to your skin.
2. Birth Control for Acne
Hormonal birth control is often used to treat persistent acne that worsens with the menstrual cycle. But not all birth control pills are created equal when it comes to skincare benefits.
Only specific combinations have been FDA-approved for acne treatment. These typically pair ethinyl estradiol with progestins like norgestimate, norethindrone acetate, or drospirenone. Together, they help regulate androgen levels—reducing oil production and breakouts.
Beyond the pill, other hormonal contraceptives like the patch and vaginal ring can offer similar skin-clearing effects. These also contain estrogen and progestin to balance hormones throughout the cycle.
For many, using hormonal birth control becomes a dual-purpose tool: effective contraception and long-term acne control. Be sure to discuss options with your healthcare provider to find the safest fit for your needs.
3. Oral Medications for Stubborn Hormonal Acne
If topical treatments aren’t enough, oral medications may be the next step—especially for moderate to severe hormonal acne.
Spironolactone is a common choice for women. Originally prescribed for high blood pressure, it works by blocking the effects of androgens like testosterone, reducing oil production.[7Cite Charny JW, Choi JK, James WD. Spironolactone for the treatment of acne in women, a retrospective study of 110 patients. Int J Womens Dermatol. 2017 Mar 13;3(2):111-115. doi: 10.1016/j.ijwd.2016.12.002.] Because of its hormone-modulating action, it’s rarely used for men due to potential side effects like breast enlargement.
In more complex cases, dermatologists may prescribe oral antibiotics like doxycycline or minocycline to fight bacteria and reduce inflammation. For severe, cystic acne that doesn’t respond to other treatments, isotretinoin (formerly sold as Accutane) may be recommended. This powerful retinoid targets all major causes of acne but requires close medical supervision due to its potential side effects.
Talk to your doctor to determine if oral medications are right for your skin and hormone profile.
Best Skincare Products for Hormonal Acne
Skincare plays a key role in managing hormonal acne—especially when paired with a healthy lifestyle. Alongside balanced nutrition, stress management, and good sleep, using the right products can help prevent flare-ups and support skin recovery.
Dermatologists recommend choosing products with anti-inflammatory, antibacterial, or oil-controlling ingredients. Some of the most effective ingredients include:
- Salicylic acid: Gently exfoliates to clear pores
- Benzoyl peroxide: Kills acne-causing bacteria
- Niacinamide: Soothes redness and helps balance oil production
Look for formulations that match your skin’s needs—especially during oily or breakout-prone phases of your cycle. The right products can make a big difference in keeping hormonal acne under control.
1. AcneFree Oil-Free Acne Cleanser

If you’re looking for a budget-friendly yet effective daily cleanser, AcneFree Oil-Free Acne Cleanser is a standout choice.
It contains 2.5% benzoyl peroxide, a clinically proven acne-fighting ingredient that kills bacteria and clears clogged pores—without being too harsh for everyday use.
This cleanser is ideal for beginners who are just starting a routine for hormonal acne. It’s gentle enough for daily cleansing but powerful enough to reduce active breakouts over time. Plus, it’s widely available and affordable, making it a smart addition to your acne care toolkit.
2. St. Ives Acne Control Tea Tree Daily Cleanser

Salicylic acid is a key ingredient in treating hormonal acne. As a beta hydroxy acid (BHA), it penetrates deep into pores to clear out excess oil and dead skin cells—two major contributors to breakouts.
Dermatologists recommend using a salicylic acid cleanser regularly, especially in the luteal phase of your cycle, when skin becomes oilier and more inflamed. Proper cleansing also helps remove dirt, sweat, and leftover makeup—preventing future blockages.
St. Ives Acne Control Tea Tree Daily Cleanser combines 2% salicylic acid with tea tree oil, a natural anti-inflammatory and antibacterial agent. This pairing makes it ideal for managing mild to moderate acne—like small whiteheads or clogged pores that tend to show up before your period.
Its gentle yet effective formula is perfect for daily use and works well as a preventive step in your skincare routine—especially if you’re prone to hormonal breakouts.
3. Dr. Loretta Concentrated Firming Serum

Retinoids are powerhouse ingredients when it comes to both acne and aging. The over-the-counter form, retinol, helps boost cell turnover, unclog pores, and fade dark spots from past breakouts.
Experts often recommend retinol for those dealing with hormonal acne and skin texture issues. It not only targets active acne but also improves skin tone and smoothness over time.
Dr. Loretta Concentrated Firming Serum contains 0.5% retinol—an ideal strength for beginners. It offers visible results without being too harsh, though those with very sensitive skin should patch-test first.
Apply retinol at night and follow with a calming moisturizer. Since retinoids increase sun sensitivity, always pair with sunscreen during the day to protect your skin and boost results.
4. AcneFree Adapalene Gel

Adapalene is a dermatologist-favorite retinoid that effectively treats hormonal acne. Unlike older retinoids, it’s more stable and better tolerated—making it suitable for most skin types, including sensitive skin.
Adapalene helps regulate skin cell turnover, prevents clogged pores, and reduces inflammation—three key factors behind hormonal breakouts.
AcneFree Adapalene Gel contains 0.1% adapalene and is available over the counter. It’s clinically proven to treat and prevent acne while being budget-friendly and accessible.
If you’re dealing with frequent breakouts or deep, stubborn pimples, adding adapalene to your nighttime routine could make a major difference. Just remember to ease into usage, hydrate well, and always use SPF daily to protect your progress.






 Acne
Acne Anti-Aging
Anti-Aging Business
Business Digital Marketing
Digital Marketing Economics
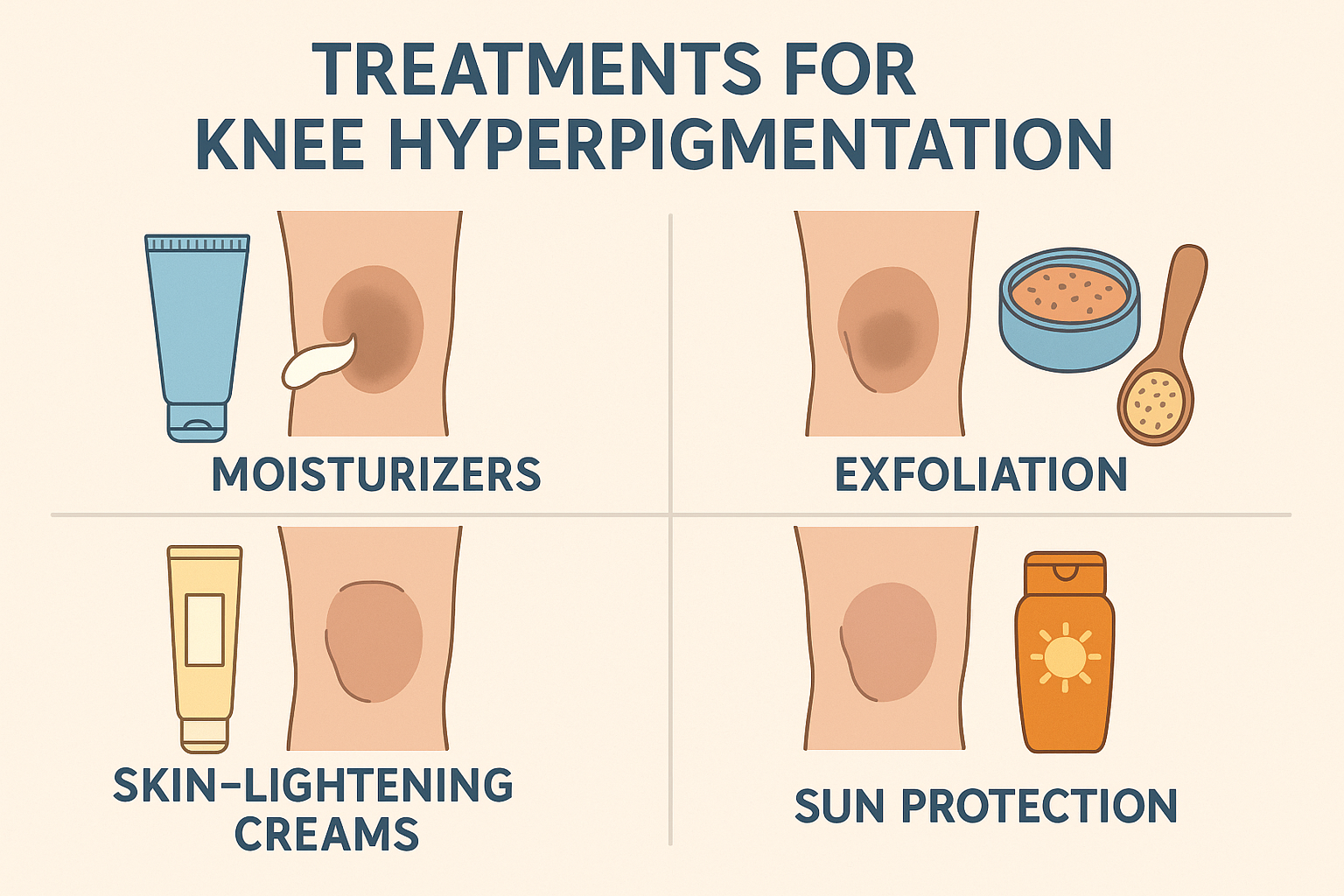
Economics Exfoliation
Exfoliation Hair Removal
Hair Removal Movies
Movies Personal Finance
Personal Finance Websites
Websites