Bumps on Your Legs? They Might Not Be Pimples
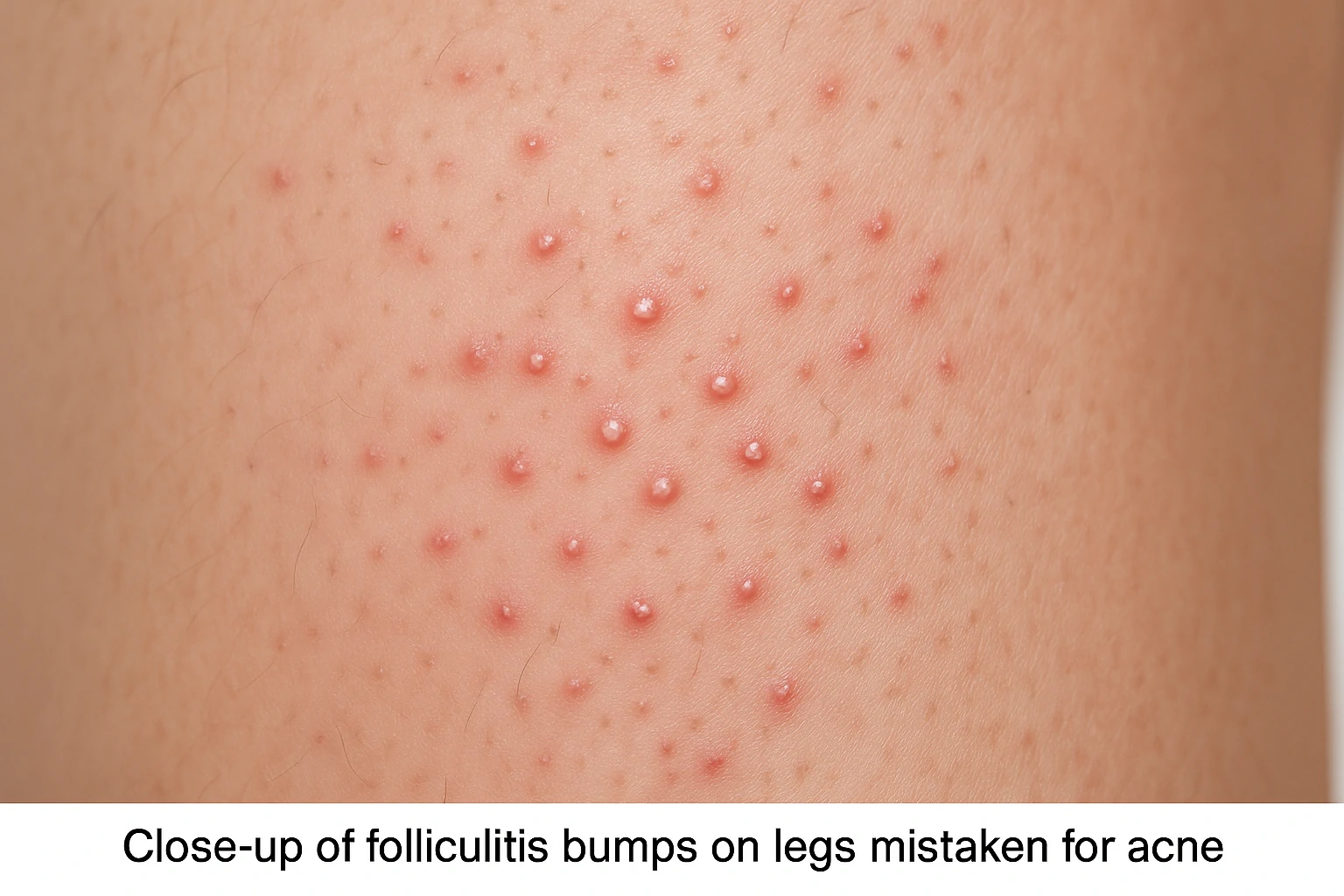
Noticing small, red, pimple-like bumps on your legs? You might assume they’re acne—but in most cases, they’re not. Dermatologists say it’s actually rare for true acne to form on the legs.
The most likely culprit is folliculitis, a common condition where hair follicles become inflamed. This often happens when fine leg hairs get irritated or blocked, triggering redness, swelling, and sometimes pus.
Folliculitis can look like acne, especially when bumps are filled with yellowish fluid or develop crusts. If these appear suddenly or in clusters, it may feel alarming. According to Dr. Whitney Bowe, a board-certified dermatologist, “Folliculitis is easily mistaken for breakouts, but the root cause and treatment are different.”
The good news? Mild cases often resolve on their own. But identifying the real cause and knowing how to prevent it makes a huge difference. With proper care, you can keep your legs smooth, irritation-free, and confident all summer long.
Common Triggers: What Causes Folliculitis?
Folliculitis happens when hair follicles become inflamed or infected—and everyday habits could be to blame. Common triggers include tight clothing, trapped sweat, heat, friction, or shaving.
Wearing sweaty gym clothes too long, using dull razors, or staying in hot, humid conditions can create the perfect environment for bacteria or yeast to grow. Even ingrown hairs can lead to this type of irritation.
Thankfully, many of these triggers are avoidable. Dermatologists recommend switching to breathable fabrics like cotton, changing out of workout clothes promptly, and being gentle during shaving. Using non-comedogenic products that don’t clog pores also reduces risk.
By understanding what’s causing the irritation, you can adjust your skincare and clothing habits to prevent folliculitis before it starts—especially in high-friction areas like thighs, buttocks, and lower legs.
Smart Skincare: How to Prevent Folliculitis
Preventing folliculitis starts with keeping your skin clean, cool, and calm. One of the best moves? Avoid tight or synthetic clothing, especially during workouts. Loose, cotton fabrics let your skin breathe and reduce heat and sweat buildup.[1Facial bacterial infections: Folliculitis. Clinics in Dermatology. Volume 32, Issue 6. 2014. doi: 10.1016/j.clindermatol.2014.02.009.]
After exercising or sweating, shower as soon as possible and change into fresh clothes. This helps remove bacteria, oil, and dirt that could trigger follicle inflammation.
Shaving is another common trigger. Always shave in the direction of hair growth using a sharp razor and hydrating shave gel. Don’t shave over irritated skin. Afterward, gently exfoliate and moisturize. Dermatologists like Dr. Sandra Lee recommend products containing colloidal oatmeal to soothe post-shave redness.
A top pick? Aveeno Daily Moisturizing Lotion—widely praised for calming sensitive skin while keeping it hydrated.
Building a few simple habits can go a long way in keeping your skin clear and preventing recurring bumps.
Effective Treatments: How to Get Rid of Folliculitis
Treating folliculitis depends on the severity, but most mild cases respond well to over-the-counter skincare. Cleansers with salicylic acid or benzoyl peroxide help clear blocked follicles and reduce bacteria.
A standout option is PanOxyl Acne Foaming Wash, which contains 10% benzoyl peroxide—strong enough to fight germs, yet gentle enough for body use.
For more inflamed cases, dermatologists may recommend a topical antibiotic like clindamycin lotion, applied twice daily. If that doesn’t work or the infection spreads, oral antibiotics might be prescribed.
Some chronic cases—especially those triggered by shaving—might benefit from laser hair removal, which reduces hair regrowth and prevents irritation. Dr. Joshua Zeichner notes that “laser treatments are a smart long-term option for patients with recurring folliculitis caused by ingrown hairs.”
Whatever the cause, tailored treatment guided by a professional can speed up healing and prevent flare-ups.
Types of Folliculitis and How to Spot Them
Folliculitis isn’t one-size-fits-all. Knowing the type you’re dealing with is key to choosing the right treatment—and avoiding what could make it worse.
Here are the most common types:
- Bacterial folliculitis: Caused by bacteria like Staphylococcus aureus. It presents as red, pus-filled bumps and may feel sore.
- Fungal folliculitis (Pityrosporum): Triggered by yeast, it usually appears on the back or chest and tends to itch intensely.
- Pseudofolliculitis barbae: Often seen in people who shave frequently. It’s caused by ingrown hairs and commonly affects beards or bikini lines.
- Irritant folliculitis: Not caused by infection, but by friction or poor shaving tools.
According to Dr. Mona Gohara, “Treating fungal folliculitis with antibiotics can make things worse—so getting an accurate diagnosis is crucial.”
If bumps don’t improve with basic care, see a dermatologist. They can determine the cause and customize a plan that gets your skin back on track—safely and effectively.
Is Folliculitis Contagious?
Is folliculitis contagious? The answer depends on the cause. Not all types are infectious, but some—especially those triggered by bacteria or fungi—can spread to others.
Bacterial folliculitis caused by Staphylococcus aureus can be passed through direct skin contact or shared personal items like towels, razors, or tight clothing. Fungal folliculitis can also spread in warm, damp environments like public gyms or swimming pools.
However, non-infectious types, such as pseudofolliculitis barbae (caused by ingrown hairs) or irritation from shaving and friction, are not contagious since they’re not driven by microorganisms.
To prevent spreading infectious folliculitis, dermatologists recommend good hygiene habits—don’t share personal items, always shower after sweating, and change into clean clothes immediately.
If you’re experiencing repeated breakouts or symptoms on multiple areas of the body, consult a dermatologist. Early diagnosis not only helps with faster healing but also prevents transmission to others, especially in close-contact environments.
Skincare Ingredients to Avoid During Folliculitis Flares
When you’re dealing with folliculitis, choosing the right skincare is essential. Some ingredients can worsen irritation or clog follicles—especially in sensitive or sweaty areas like legs, back, or underarms.
Dermatologists suggest avoiding the following:
- Mineral oil and lanolin: These occlusive agents can trap bacteria and block follicles.
- Denatured alcohol: Often in toners, it can dry and irritate inflamed skin.
- Synthetic fragrance: Common in lotions and cleansers, it increases the risk of redness or allergic reactions.
- Heavy silicones (e.g., dimethicone): While generally safe, overuse may contribute to clogged pores on already-reactive skin.
Instead, look for fragrance-free, water-based, and non-comedogenic formulas. Soothing ingredients like colloidal oatmeal or niacinamide help calm irritation while supporting skin repair.
If unsure about a product, it’s best to consult a dermatologist to ensure it’s suitable for your skin condition.
Dermatologist-Recommended Skincare for Folliculitis-Prone Skin
Caring for folliculitis-prone skin means using products that cleanse gently, prevent bacterial buildup, and soothe irritation—without clogging your pores.
Here are expert-approved, non-irritating options:
- CeraVe Hydrating Cleanser: Soap-free, fragrance-free, and packed with ceramides to strengthen the skin barrier—great for daily use on face and body.
- PanOxyl Acne Foaming Wash (10% Benzoyl Peroxide): A powerful antibacterial cleanser for body acne and folliculitis, especially effective on legs and back.
- Aveeno Daily Moisturizing Lotion: Contains colloidal oatmeal to calm redness and irritation without added fragrance or heavy oils.
- La Roche-Posay Lipikar Balm AP+M: A lightweight body moisturizer with niacinamide and shea butter, ideal for dry, irritated skin.
Look for labels like non-comedogenic, hypoallergenic, and fragrance-free to minimize the risk of flare-ups. And if your skin reacts unexpectedly, stop using the product and seek advice from a qualified skin specialist.






 Acne
Acne Anti-Aging
Anti-Aging Business
Business Digital Marketing
Digital Marketing Economics
Economics Exfoliation
Exfoliation Hair Removal
Hair Removal Movies
Movies Personal Finance
Personal Finance Websites
Websites