How to Reduce Acne Redness Fast and Effectively

Acne is one of the most common skin concerns, affecting over 50 million people worldwide each year.[1American Academy of Dermatology Association. Skin conditions by the numbers.] While pimples themselves can be frustrating, the lingering redness that often remains afterward is just as troubling—especially for those with deeper skin tones where it may evolve into post-inflammatory hyperpigmentation (PIH).
This redness occurs as part of the body’s natural inflammatory response. Blood flow increases to the irritated area, making the skin appear red, swollen, and sometimes tender. Even with makeup, covering it can be a challenge.
Experts agree that identifying the root cause of acne redness is crucial before choosing the right treatment. In this guide, we’ll explore fast, dermatologist-approved methods to calm inflammation, fade redness, and help your skin recover smoothly—without triggering further irritation.
What Exactly Is Acne Redness?
Acne redness is not an active breakout—it’s a leftover sign of inflammation.[2Healthline: How to Get Rid of Redness from Pimples and Acne.] Dermatologists explain that this discoloration stems from skin trauma, often worsened by picking or popping pimples. This can damage surrounding tissues and trigger increased melanin production, leading to red, brown, or purplish marks.
Another factor is dilated blood vessels. As your body sends extra oxygen and nutrients to heal the area, those vessels expand, causing visible redness that may last 4 to 12 weeks.
Unlike scars, these marks are part of your skin’s recovery. Their duration depends on how intense the original inflammation was and how well your skin regenerates. With the right care, this redness can fade much faster—especially if you avoid further irritation.
8 Effective Ways to Reduce Red Acne Marks
1. Stop Touching or Picking Your Pimples
One of the most important rules: hands off your face. Picking at acne slows healing, spreads bacteria, and increases the risk of dark spots or permanent scars.
Instead, use an ice cube wrapped in a clean cloth and gently press it against the red area for 5–10 minutes. This helps constrict blood vessels, instantly reducing redness and swelling.
Follow up with a spot treatment containing salicylic acid, benzoyl peroxide, or sulfur—ingredients known for their acne-fighting and calming effects.
To resist the urge to touch, some experts suggest writing a “no-pick pledge” or setting reminders to build discipline. The less you touch, the faster your skin will calm down.
2. Try Anti-Inflammatory Skincare and Diet
Tackling acne redness requires both topical care and internal support. Use products with anti-inflammatory ingredients like niacinamide or green tea extract to soothe the skin barrier and speed up recovery. A dermatologist-recommended product like Epionce Lytic is often praised for its gentle yet effective anti-inflammatory action.
Equally important is what you eat. A high-sugar, processed-food-heavy diet can fuel inflammation. Experts advise avoiding sugary drinks, white bread, spicy foods, and excess dairy.[3Minihane AM, Vinoy S, Russell WR, Baka A, Roche HM, Tuohy KM, Teeling JL, Blaak EE, Fenech M, Vauzour D, McArdle HJ, Kremer BH, Sterkman L, Vafeiadou K, Benedetti MM, Williams CM, Calder PC. Low-grade inflammation, diet composition and health: current research evidence and its translation. Br J Nutr. 2015 Oct 14;114(7):999-1012. doi: 10.1017/S0007114515002093.]
Boost your gut health with probiotics or fermented foods like kimchi and kefir. Studies show that a healthy gut microbiome can reduce systemic inflammation, helping calm your skin from the inside out.
3. Never Skip Sunscreen—Even Indoors
Sunscreen is non-negotiable when treating red acne marks. UV exposure can worsen inflammation and lead to long-lasting discoloration.[4Cleveland Clinic. Acne scars: management and treatment. Updated June 23, 2020.]
Even cloudy days or indoor light sources can trigger pigmentation. That’s why dermatologists recommend using a broad-spectrum sunscreen with at least SPF 30 daily—regardless of the weather.
By blocking harmful UV rays, sunscreen protects your skin’s healing process and prevents marks from becoming darker or more stubborn. It also keeps your overall skin tone more even and balanced over time.
4. Drink Green Tea for Skin-Calming Benefits
Green tea isn’t just a healthy drink—it’s a powerful skin ally. Dermatologists highlight its rich polyphenols, especially catechins, which have potent antioxidant and anti-inflammatory properties. These compounds help soothe red, irritated skin caused by acne flare-ups.[5OyetakinWhite P, Tribout H, Baron E. Protective mechanisms of green tea polyphenols in skin. Oxid Med Cell Longev. 2012;2012:560682. doi:10.1155/2012/560682.]
Drinking freshly brewed green tea daily may help reduce inflammation from within, making it a smart addition to your skincare routine. For added hormonal balance, spearmint tea is also recommended, especially for those dealing with hormonal acne. Some studies suggest that spearmint may help regulate androgens, a hormone linked to breakouts.
While not a quick fix, green tea is a gentle, natural option that supports clearer, calmer skin over time. Combining it with consistent topical care can give your skin a much-needed healing boost—one sip at a time.
5. Use Gentle Brightening and Exfoliating Products
To fade acne redness and post-breakout marks, use skincare products that brighten the skin and gently exfoliate. Experts recommend non-irritating fading gels formulated with ingredients like white tea extract, lactic acid, and amino acids. These support skin renewal without causing further sensitivity.
White tea calms inflammation, while mild acids encourage cell turnover, helping discolored spots fade more quickly. Look for hydroquinone-free brightening creams, which are safer for long-term use, especially on skin prone to post-inflammatory hyperpigmentation (PIH).
Consistency is key—visible improvements often start within a few weeks of regular use. The right products can help restore an even skin tone while protecting your skin barrier.
6. Consider Microneedling for Deep Redness and Scars
Microneedling is a minimally invasive treatment designed to smooth acne scars and reduce discoloration. This procedure uses ultra-fine needles to create micro-injuries on the skin’s surface, which stimulates natural collagen production.[6The American Association of Dermatology. Acne Scars: Diagnosis and Treatment.]
Collagen helps repair uneven texture and gradually fades hyperpigmented marks. According to dermatology associations, microneedling can be especially effective for atrophic scars and post-acne redness.
Most patients need 3–6 sessions spaced several weeks apart. While it’s an investment, many experts view it as a long-term solution when paired with proper aftercare, including soothing serums and sunscreen.
If you’re looking for visible texture improvement without aggressive resurfacing, microneedling offers a balanced, science-backed approach.
7. Explore Laser Treatments for Stubborn Redness
Laser therapy is one of the most effective options for persistent acne redness. It targets dilated blood vessels beneath the skin’s surface—the root of lingering red tones after breakouts.
Popular technologies include vascular lasers, IPL (Intense Pulsed Light), and BBL (Broadband Light). These treatments reduce redness and improve overall skin tone by collapsing overactive blood vessels.
For deeper skin tones, lasers like the 1064nm Nd:YAG are preferred for safety and reduced risk of pigmentation changes. Devices such as ClearSilk by Sciton are commonly recommended by dermatologists for treating acne-related discoloration without damaging surrounding tissue.
Though costlier than topical options, laser therapy delivers fast, noticeable results—often with minimal downtime when using modern non-ablative systems.
8. Try LED Light Therapy for Gentle Skin Recovery
LED light therapy is a painless, non-invasive method to reduce acne-related redness. Using specific wavelengths of light, this treatment stimulates skin healing, boosts circulation, and supports collagen production—without damaging the skin.
Blue light targets acne-causing bacteria, while red light calms inflammation and accelerates cellular repair. Over time, consistent sessions can help minimize redness, improve skin texture, and prevent new breakouts.
You can receive LED therapy at professional clinics or invest in at-home devices like LED masks or handheld tools. While not a quick cure, this therapy offers a gentle, effective supplement to your skincare routine—especially for sensitive or reactive skin types.
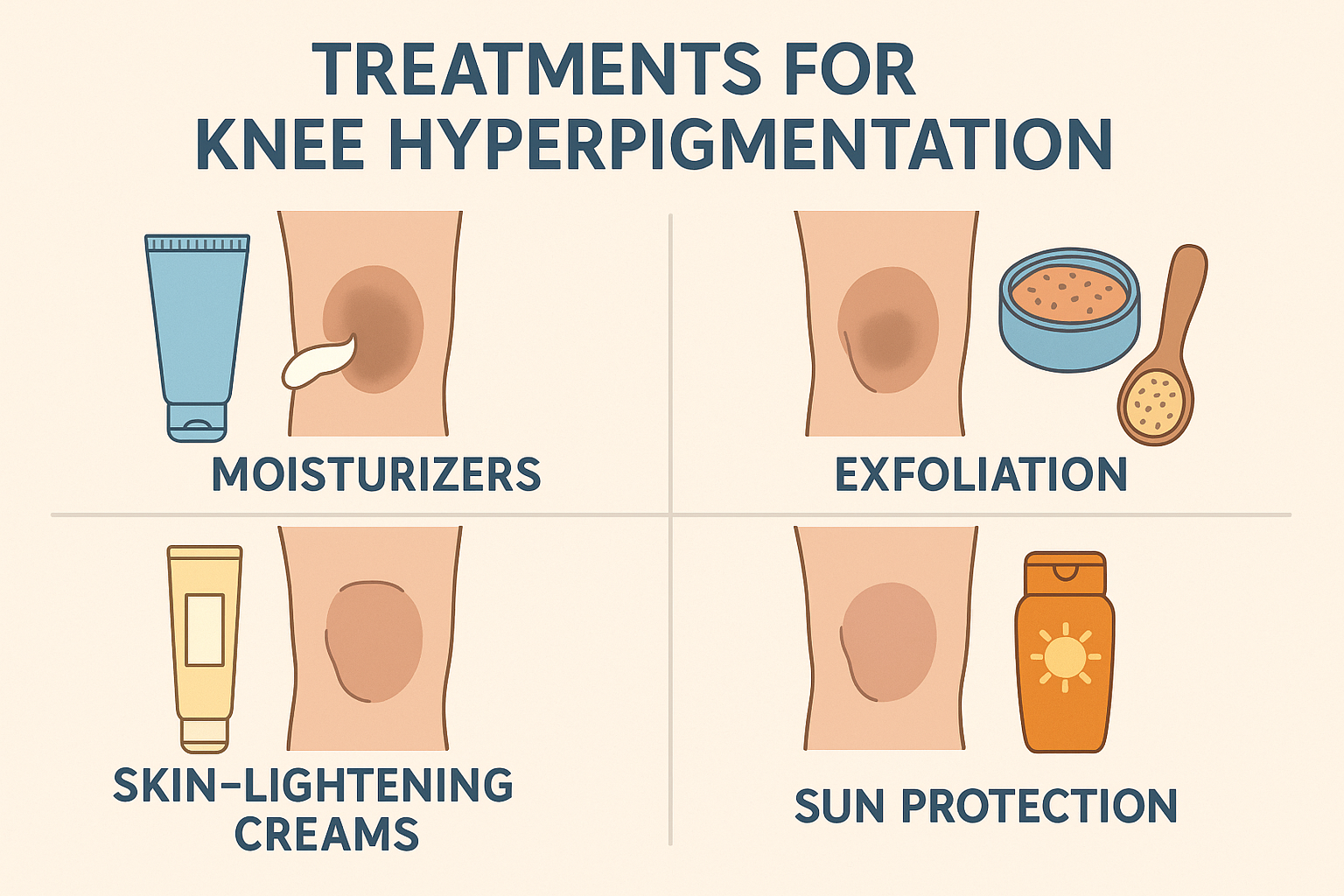
Redness vs Hyperpigmentation: What’s the Difference?
Not all acne marks are created equal. Many people assume that every leftover spot is the same, but there are two distinct conditions: post-inflammatory erythema (PIE) and post-inflammatory hyperpigmentation (PIH). Understanding the difference is key to choosing the right treatment.
PIE appears as red or purplish patches and is caused by dilated capillaries from inflammation. It’s more common in lighter skin tones and often mistaken for an active breakout. In contrast, PIH shows up as brown or dark spots, particularly in deeper skin tones, and results from excess melanin production after skin trauma.
According to dermatologists, PIE responds best to treatments that calm blood vessels—such as laser therapy or anti-inflammatory skincare—while PIH requires brightening ingredients like niacinamide, azelaic acid, or gentle retinoids.
By knowing the type of mark you’re dealing with, you can avoid ineffective products and focus on what your skin really needs to heal.
Top Ingredients to Calm Acne Redness
To truly reduce acne redness, gentle cleansers alone won’t cut it. You’ll need active ingredients that target inflammation and support skin recovery. Dermatologists recommend the following top ingredients:
- Niacinamide (Vitamin B3): Calms inflammation and strengthens the skin barrier.
- Centella Asiatica: A healing botanical that soothes irritation and boosts repair.
- Azelaic Acid: Fights inflammation and fades discoloration, ideal for sensitive skin.
- Green Tea Extract: A natural antioxidant that reduces redness and calms reactive skin.
- Allantoin: Softens skin and minimizes mild redness without irritation.
Choose a formula that matches your skin type—gels or serums work best for oily or sensitive skin. For long-lasting results, apply consistently and always follow with sunscreen to protect your skin during healing.
With patience and the right ingredients, visible improvements can often be seen within a few weeks.
Is It Safe to Wear Makeup on Red, Irritated Skin?
Wearing makeup on red, post-acne skin is safe—as long as you choose the right products and prep your skin properly. Dermatologists emphasize using non-comedogenic, alcohol-free formulas that won’t clog pores or worsen irritation.
Opt for lightweight foundations, BB creams, or cushions that feel breathable. To neutralize redness, apply a green color corrector under your base makeup—it helps cancel out red tones without layering on heavy product.
Start with clean, moisturized skin and don’t skip sunscreen. A well-hydrated skin barrier helps makeup sit better and reduces the risk of further irritation.
Most importantly, always remove your makeup thoroughly before bed. Sleeping in makeup can clog pores, trigger breakouts, and delay your skin’s recovery. With the right routine, you can wear makeup confidently—even while your skin is healing.






 Acne
Acne Anti-Aging
Anti-Aging Business
Business Digital Marketing
Digital Marketing Economics
Economics Exfoliation
Exfoliation Hair Removal
Hair Removal Movies
Movies Personal Finance
Personal Finance Websites
Websites