9 Pro Tips to Stop Excess Sweat (Dermatologist Approved)

Sweating, also known as perspiration, is a vital thermoregulatory process that helps the body maintain a stable core temperature. From a medical perspective, sweating is a sign that your internal cooling system is working efficiently. However, when sweat production exceeds what the body actually needs— a condition called hyperhidrosis—it can affect daily comfort, confidence, and social interactions.
The good news is that sweating does not have to be a constant source of stress. Completely stopping sweat is neither realistic nor healthy. Instead, the most effective approach is learning how to manage excessive sweating safely and clinically, using methods supported by dermatological science.
To help you do that, we’ve compiled expert-backed strategies straight from board-certified dermatologists. Dr. Mona Gohara, Dr. Marisa Garshick, Dr. Alicia Zalka, and Dr. Joshua Zeichner share practical, dermatologist-approved solutions—from simple lifestyle adjustments to prescription-level treatments—designed for real, everyday life.
9 Ways Dermatologists Fix Excessive Sweating Fast
These expert strategies focus on reducing sweat effectively without disrupting your skin’s natural balance. Whether you’re dealing with sweaty underarms, palms, or body folds, each method is designed to be practical, evidence-based, and easy to follow—especially if you’re new to skincare or sweat management.
1. Start the Day Dry: Build a Sweat-Smart Morning Routine
An effective sweat-control routine begins with completely dry skin. After showering, dermatologist Dr. Alicia Zalka emphasizes that drying your body thoroughly is more than a quick towel pat.
She recommends using a hair dryer on a cool setting to gently dry moisture-prone areas such as underarms, under the breasts, or skin folds. This extra step helps prevent trapped moisture, which can trigger excessive sweating and odor later in the day.
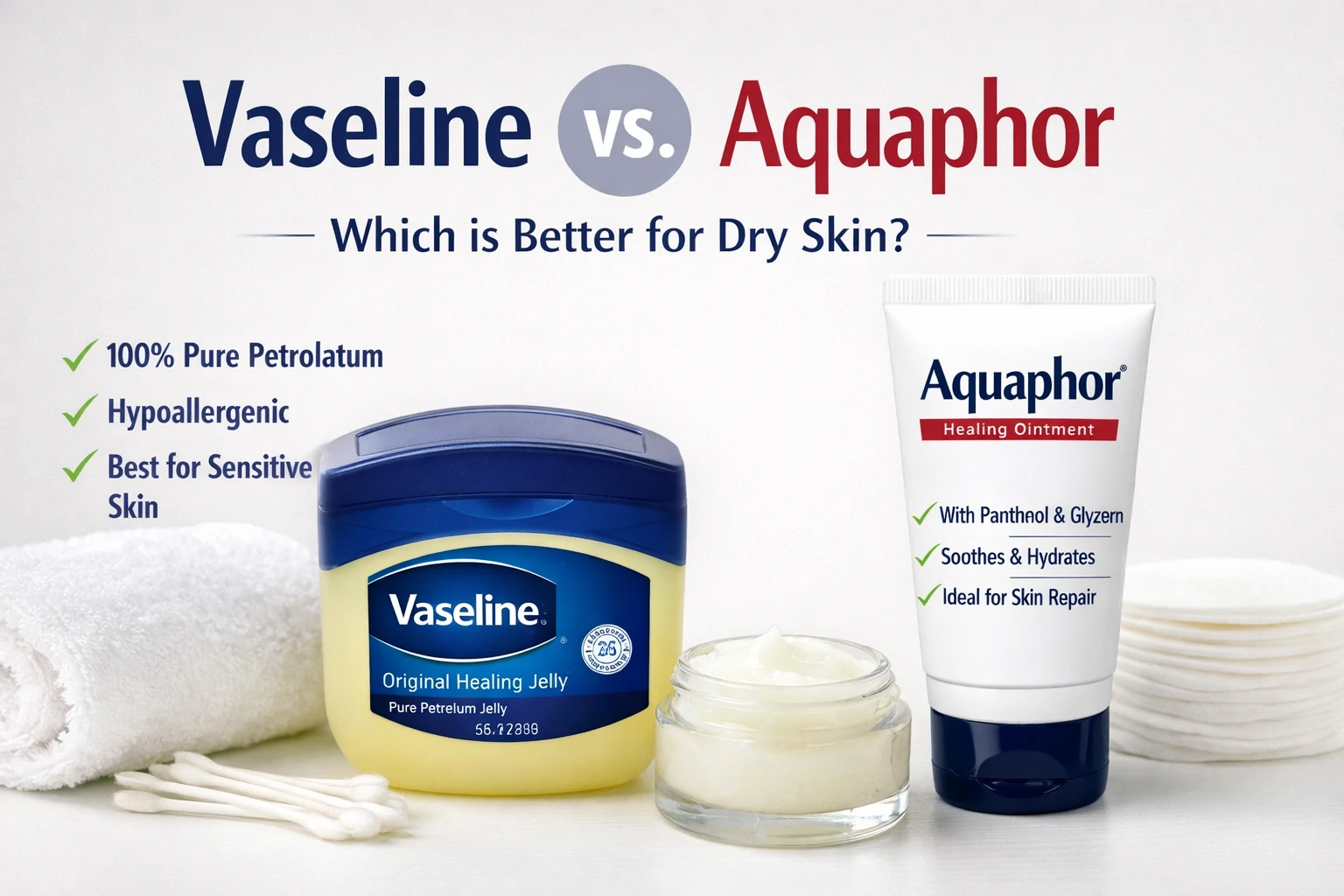
Dr. Mona Gohara offers a helpful analogy: applying antiperspirant to damp skin is like painting on a wet canvas—it simply doesn’t work as well. Residual moisture can dilute products and reduce their effectiveness. Starting your day with fully dry skin allows antiperspirants and skincare products to perform at their best, setting you up for a more comfortable, confident day ahead.
2. Cleanse Smart, Not Harsh: Protect Skin While Managing Sweat
Although sweat itself is sterile, letting it sit on the skin for too long can create an ideal environment for bacterial growth. According to dermatologist Dr. Mona Gohara, sweat buildup—especially when mixed with oil (sebum)—can encourage acne-causing bacteria such as Cutibacterium acnes, leading to body breakouts and irritation.
That’s why daily, targeted cleansing is essential for areas prone to excessive sweating, including the underarms, under the breasts, and the groin. The key is to cleanse thoroughly without stripping the skin.
Dr. Gohara recommends using a gentle yet effective cleanser that helps control bacteria while preserving the skin barrier. Products containing salicylic acid can be particularly helpful, as they provide mild chemical exfoliation to prevent clogged pores and sweat-related body acne. An example is Neutrogena Oil-Free Acne Wash, often suggested for sweat-prone skin.
When done correctly, smart cleansing supports a healthy skin microbiome, reduces odor and breakouts, and helps you manage excessive sweating—without irritation or over-drying.
3. Use an Antiperspirant—Not Just a Deodorant
Understanding the difference between deodorant and antiperspirant is a crucial step in controlling excessive sweating. While they’re often used interchangeably, they work in very different ways.
Deodorants are designed to neutralize odor, which occurs when sweat interacts with skin bacteria. However, they do not reduce sweat production. If moisture is your main concern, deodorant alone won’t be enough.
Antiperspirants, on the other hand, are specifically formulated to reduce sweat output. Dermatologist Dr. Joshua Zeichner explains that antiperspirants contain aluminum-based compounds, such as aluminum chlorohydrate. These ingredients temporarily form a gel-like plug in the sweat ducts, limiting the amount of sweat that reaches the skin’s surface.
Addressing common concerns, Dr. Zeichner emphasizes that current scientific evidence does not support a causal link between aluminum-based antiperspirants and serious conditions like breast cancer. When used as directed, antiperspirants are both effective and safe, making them a dermatologist-approved solution for managing excess sweat confidently.
4. Manage Stress Sweat on Two Fronts: Body and Mind
Not all sweat is the same. Stress-induced sweating behaves differently from heat-related sweat. Dermatologist Dr. Mona Gohara explains that stress sweat mainly comes from apocrine glands, which are concentrated in areas like the underarms and groin, rather than eccrine glands that regulate body temperature. Apocrine sweat contains more proteins and lipids, which skin bacteria break down—resulting in stronger body odor.
Because stress sweat has both physical and emotional triggers, it’s best managed using a two-pronged strategy:
- Physical defense: Antiperspirant
Consistent use of antiperspirant helps block sweat from reaching the skin’s surface. By reducing moisture, it also limits the environment bacteria need to thrive—helping control both wetness and odor. - Psychological defense: Stress reduction
Since stress sweat is driven by the sympathetic “fight-or-flight” response, calming the nervous system matters. Dr. Gohara recommends simple relaxation techniques such as deep breathing, mindfulness, or short meditation sessions to lower overall stress reactivity.
By addressing both the symptom (sweat) and the trigger (stress), this dual approach offers more effective, long-term control.
5. Apply Antiperspirant at Night for Maximum Effectiveness
If your antiperspirant isn’t delivering the results you expect, timing may be the issue. Dermatologist Dr. Marisa Garshick advises applying antiperspirant at night, just before bed, on clean and completely dry skin.
The science behind this tip is straightforward. Antiperspirants work by forming temporary plugs in sweat ducts using aluminum-based salts. At night, sweat glands are naturally less active, which allows these ingredients to penetrate the ducts more effectively. As Dr. Garshick explains, when the ducts are relatively dry, the aluminum compounds can form stronger, longer-lasting plugs.
This means that by morning, your sweat defense system is already fully activated—ready to perform throughout the day, even as your body temperature and activity level rise. Dr. Mona Gohara also supports nighttime application, especially before important events, to ensure optimal protection against excessive sweating when it matters most.
6. Consider Botox for Excessive Sweating (Hyperhidrosis Treatment)
For people dealing with severe excessive sweating, medically known as hyperhidrosis, botulinum toxin type A (Botox) can be a highly effective treatment option. Dermatologist Dr. Marisa Garshick notes that Botox is often recommended when prescription-strength or over-the-counter antiperspirants fail to provide adequate relief. Common treatment areas include the underarms, palms, soles of the feet, and even the scalp.
From a medical standpoint, Botox works by blocking nerve signals that trigger sweat production. As Dr. Garshick explains, it inhibits neurotransmitters released by the sympathetic nervous system, preventing eccrine sweat glands from receiving the signal to activate. Without this signal, sweat production in the treated area is significantly reduced.
While Botox is not typically a first-line treatment, its impact on quality of life can be substantial. Dr. Mona Gohara emphasizes that many patients experience truly transformative results—no longer needing to change clothes frequently or avoid social situations. The effects generally last several months, making Botox a reliable, dermatologist-approved option for long-term sweat control.
7. Choose Breathable Fabrics and Sweat-Smart Timing
Managing excessive sweat isn’t just about skincare—it also involves smart clothing choices. Dermatologist Dr. Mona Gohara highlights that fabric selection plays a major role in how sweat feels and looks throughout the day.
- Prioritize breathable, moisture-wicking materials
Natural fabrics like cotton allow better airflow and absorb moisture more effectively. Technical, moisture-wicking fabrics designed for activewear can also help pull sweat away from the skin and speed up evaporation. In contrast, tight-fitting or heat-trapping materials—especially non-technical synthetic fabrics—can worsen overheating and increase sweat production. - Use color strategy to camouflage sweat marks
Color matters more than most people realize. According to Dr. Joshua Zeichner, very light or very dark colors are best at hiding sweat stains.
Best choices: white, black, navy
Colors to avoid: mid-tones like gray or light blue, which show sweat most easily
By combining breathable fabrics with thoughtful color choices, you can manage both the comfort and appearance of sweating more confidently throughout the day.
8. When to See a Board-Certified Dermatologist
If everyday sweat-management strategies—such as proper antiperspirant use and lifestyle adjustments—aren’t enough, it may be time to seek professional help. Dr. Alicia Zalka advises consulting a board-certified dermatologist when sweating feels uncontrollable and begins to interfere with daily activities, work, or social confidence.
Excessive sweating without obvious triggers like heat or exercise may indicate hyperhidrosis, a medical condition characterized by chronic overproduction of sweat. Although not extremely common, hyperhidrosis requires targeted medical care. Dr. Zalka explains that treatment may involve prescription medications (topical or oral) or in-office procedures that are only available through a qualified dermatologist.
To put it simply, Dr. Mona Gohara describes hyperhidrosis as a body stuck in permanent “fight-or-flight” mode. The sympathetic nervous system keeps activating sweat glands as if you’re facing danger—when you’re not. Getting an accurate diagnosis is essential, as it opens the door to effective treatments that can significantly improve comfort, confidence, and overall quality of life.
9. Explore Prescription Treatments for Long-Term Sweat Control
Once hyperhidrosis is formally diagnosed, dermatologists can tailor prescription treatments based on severity and affected areas.
- Oral (systemic) medications
Dr. Mona Gohara explains that medications such as glycopyrrolate (e.g., Robinul) work systemically as anticholinergics. They block acetylcholine, the chemical messenger that activates sweat glands. Oral therapy is particularly helpful for people with generalized excessive sweating, rather than sweat limited to one area. - Prescription topical treatments
Dermatologists may also prescribe stronger topical options, including anticholinergic creams or medicated wipes. These treatments reduce sweat production directly at the source and are useful for targeted areas. - Clinical-strength prescription antiperspirants
Newer FDA-approved options are also available. Dr. Joshua Zeichner highlights Sofdra, a prescription antiperspirant gel approved for underarm hyperhidrosis. It works by interrupting nerve signals that overstimulate sweat glands, offering a targeted, safe, and effective solution.
With the right prescription plan, long-term sweat control is achievable—and often life-changing.
Iontophoresis: A Non-Invasive Solution for Sweaty Hands and Feet
For people with localized hyperhidrosis, especially affecting the palms (palmar) and soles (plantar), iontophoresis offers a proven, non-invasive treatment option. This therapy is widely recommended by dermatologists when standard antiperspirants fail to reach or adequately control sweat in these hard-to-treat areas.
Iontophoresis works by delivering a low-intensity electrical current through water while the hands or feet are submerged. The current—typically mild and well tolerated—helps temporarily block sweat ducts, reducing sweat output in the treated area. Although the exact mechanism is still being studied, experts believe charged ions in the water create a functional barrier that limits sweat release.
Initial treatment usually requires several sessions per week. According to Dr. Marisa Garshick, once dryness improves, most patients can transition to maintenance sessions tailored to their needs. One major advantage is convenience: with a dermatologist’s guidance, iontophoresis can be safely performed at home using a prescribed medical device, giving patients effective control without injections or systemic medication.
Diet and Sweating: Foods That Trigger or Calm Excess Sweat
Diet plays a meaningful role in sweat regulation, as certain foods and beverages can directly stimulate sweat production. Understanding how nutrition affects the body’s thermoregulation system can help reduce excessive sweating episodes.
Common dietary sweat triggers include:
- Spicy foods: Compounds like capsaicin trick nerve receptors into sensing heat, activating the body’s cooling response—sweating.
- Caffeine and alcohol: Both stimulate the sympathetic nervous system, increasing heart rate and body temperature, which in turn activates sweat glands.
On the other hand, some foods help cool the body from within. Focus on water-rich fruits and vegetables such as watermelon and cucumber, which support hydration and heat regulation. Adequate magnesium intake is also important, as this mineral helps regulate nerve signaling and body temperature.
By limiting dietary triggers and prioritizing calming, hydrating foods, you support sweat management from the inside—complementing topical and medical treatments for more balanced, long-term control.
Permanent Medical Solutions: Understanding miraDry and ETS Procedures
For patients seeking a long-term or permanent solution to underarm hyperhidrosis, especially after prescription antiperspirants have failed, advanced medical procedures may be appropriate. One of the most established options is miraDry, a non-surgical, FDA-approved treatment designed to permanently reduce underarm sweat, odor, and even hair growth.
miraDry works by delivering controlled electromagnetic (thermal) energy to the underarm area. Dermatologist Dr. Mona Gohara explains that this heat selectively targets and destroys both eccrine and apocrine sweat glands within the dermal layer. Because sweat glands do not regenerate, the reduction achieved with miraDry is considered permanent.
The procedure typically takes about one hour and is performed in a dermatologist’s office under local anesthesia to ensure comfort. Dr. Alicia Zalka highlights that miraDry offers high effectiveness with minimal downtime—most patients resume normal activities quickly. In many cases, just one or two sessions are enough to achieve a significant and lasting reduction in underarm sweating, making miraDry a reliable option for those seeking freedom from chronic sweat concerns.
Note: In very select cases, a surgical option called Endoscopic Thoracic Sympathectomy (ETS) may be discussed, but due to its invasive nature and potential side effects, it is generally reserved for severe cases and considered only after all other treatments have been exhausted.





 Acne
Acne Anti-Aging
Anti-Aging Business
Business Digital Marketing
Digital Marketing Economics
Economics Exfoliation
Exfoliation Hair Removal
Hair Removal Movies
Movies Personal Finance
Personal Finance Websites
Websites