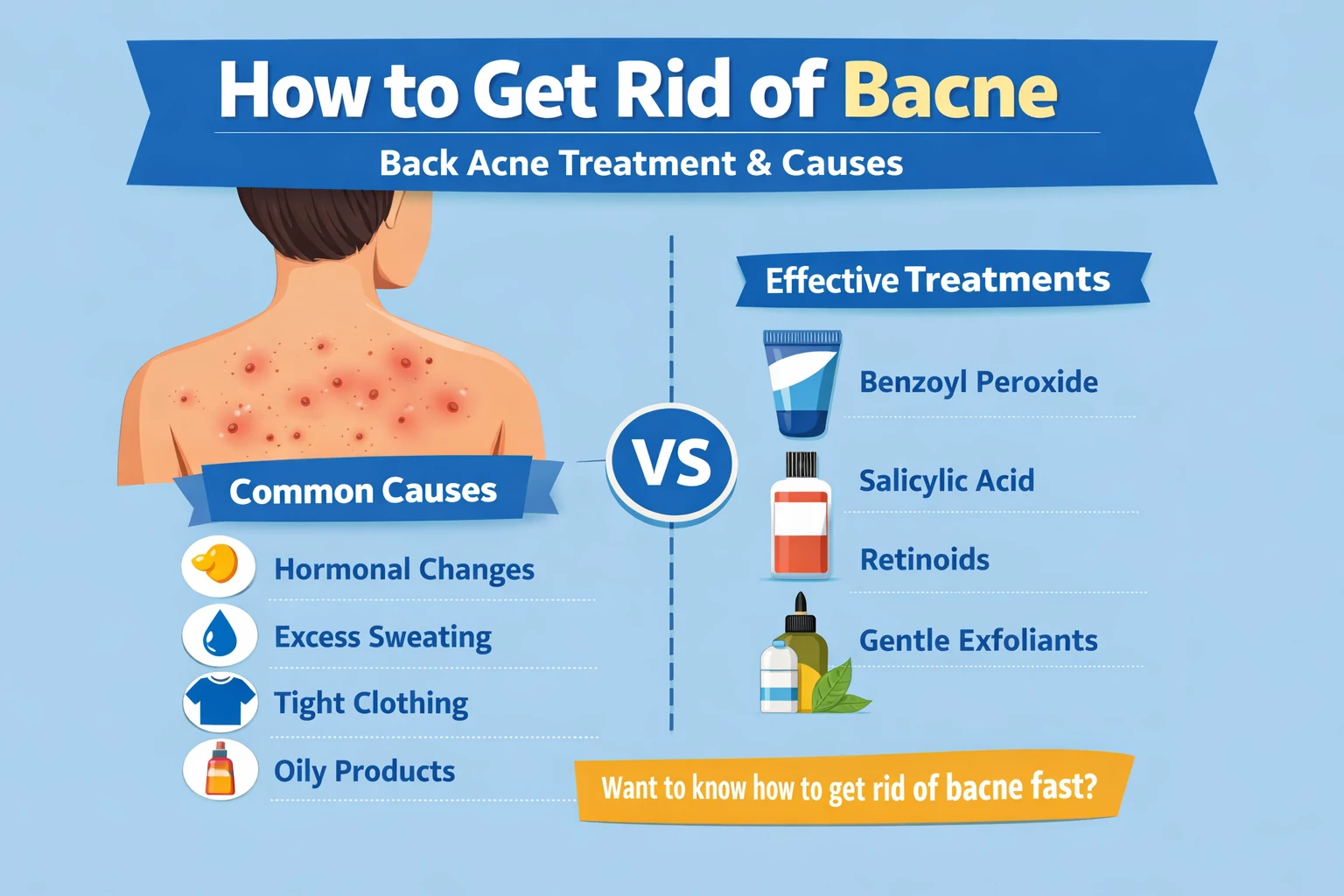
How to Get Rid of Bacne: Causes and Effective Treatments
Facial acne is often easier to manage because most people already have a basic skincare routine for it. Bacne—acne on the back—is different. It tends to be overlooked, harder to reach, and more likely to worsen before proper treatment begins.
Back acne is not just a cosmetic concern. Bacne can cause inflammation, discomfort, and long-term marks that affect confidence, especially in hot weather or when wearing open-back clothing. The back is frequently exposed to sweat, friction from clothing, and residue from body care products, all of which can clog pores and trigger breakouts.
Understanding bacne is a crucial first step toward effective treatment. This includes knowing its biological causes, how it differs from facial acne, and which treatments are both realistic and dermatologist-approved. Based on modern dermatological principles and clinical insights from board-certified dermatologists Dr. Richard Bottiglione and Dr. Hannah Kopelman, this guide focuses on practical, evidence-based strategies to help clear bacne safely and sustainably—without overcomplicating your skincare routine.
Acne Explained: What Happens Beneath the Skin
Acne is an inflammatory skin condition that develops when hair follicles become clogged with excess sebum (natural skin oil) and dead skin cells. This blockage creates an ideal environment for acne-causing bacteria, leading to inflammation and visible breakouts.
Although acne is most common on the face due to a higher concentration of oil glands, it frequently appears on the back, chest, and shoulders. These areas also produce significant amounts of sebum and are often exposed to sweat and friction, increasing the risk of clogged pores.[1Branch NSC and O. Acne. National Institute of Arthritis and Musculoskeletal and Skin Diseases.]
Clinically, acne presents in several forms depending on depth and severity. Common types include open and closed comedones (blackheads and whiteheads), inflamed papules, pus-filled pustules, firm nodules, and deep, painful cystic acne. Bacne often involves deeper, more inflamed lesions, which can make treatment more challenging and increase the risk of scarring.
Recognizing these basic acne mechanisms helps guide more effective and targeted bacne treatment strategies.
Understanding Bacne: Why Back Acne Can Be Tougher
Bacne, or back acne, refers to pimples and inflammation appearing on the back. Medically, its formation is similar to facial acne, but the back’s skin characteristics often make it more severe. According to Dr. Hannah Kopelman, the back has thicker skin and denser sebaceous glands, increasing the likelihood of clogged pores. As a result, lesions may be larger, redder, and more painful than typical facial acne.
Bacne manifests in several forms: blackheads and whiteheads, inflamed papules, pus-filled pustules, and deep nodules or cysts. Dr. Richard Bottiglione highlights that excess sweat, trapped oil, and friction from clothing further aggravate blocked pores and promote bacterial growth. Unlike facial acne, bacne is harder to treat because the back is difficult to reach, clean, and monitor regularly.
Recognizing the unique traits of bacne is essential for choosing effective and realistic treatment strategies. From selecting the right cleansers to avoiding friction-inducing clothing, understanding how bacne develops helps you target both prevention and therapy without unnecessary trial and error.
Causes of Back Acne: Internal and External Triggers
Back acne doesn’t appear randomly; it results from a mix of internal and external factors. The back has large, active sebaceous glands, making it prone to clogged pores if not cared for properly.
Common bacne triggers include:
- Excess sebum production – Too much natural oil mixes with dead skin cells and bacteria, causing pore blockage and inflammation.
- Hormonal fluctuations – Puberty, pregnancy, or menstrual cycles can increase oil gland activity.
- Sweat and hygiene – Sweat left on the skin after exercise can worsen pore blockages.
- Friction and pressure – Tight clothing, sports bras, or backpack straps irritate the skin and induce acne mechanically.
- Hair and body products – Residue from shampoo, conditioner, or styling products can clog pores.
- Genetics, diet, bacteria, and stress – Family history, skin bacteria, high sugar intake, and chronic stress can exacerbate bacne.
Identifying these triggers is key to effective prevention and treatment, helping you reduce outbreaks and maintain clearer, healthier back skin.
Risk Factors for Back Acne: Who Is Most Vulnerable
Back acne is influenced not only by skincare habits but also by specific risk factors that increase susceptibility. Dr. Hannah Kopelman notes that these factors can affect hormone balance, oil production, and the skin’s inflammatory response, making some individuals more prone to bacne than others.
Common risk factors include:
- Age – Teenagers and young adults often experience bacne due to hormonal fluctuations that boost sebum production.
- Family history – Genetics play a key role; if back acne is common in your family, your risk is higher.
- Lifestyle – Chronic stress, high-sugar diets, poor nutrition, and inconsistent skincare can aggravate back acne.
- Physical activity and daily habits – Intense exercise, excessive sweating, friction from clothing or sports gear, and use of comedogenic skin or hair products can trigger breakouts.
Understanding these risk factors early allows for targeted preventive measures, reducing the likelihood of severe bacne and supporting healthier skin over time.
Prevention and Treatment of Back Acne
Preventing Back Acne
Preventing bacne centers on keeping the skin clean, minimizing pore blockage, and reducing irritation. Small daily adjustments can make a significant difference in back skin health.
Effective preventive steps include:
- Regular cleansing – Use gentle cleansers to remove sweat, oil, and dirt without stripping the skin’s protective barrier.
- Exfoliation – Light exfoliation prevents dead skin buildup that can clog pores; avoid over-exfoliating to prevent irritation.
- Showering after sweating – Cleaning the skin promptly after exercise prevents sweat and bacteria from lingering.
- Choosing the right clothing – Loose, breathable fabrics that wick sweat help maintain dry, comfortable skin.
- Using non-comedogenic products – Skincare and haircare products that do not clog pores reduce acne risk.
- Maintaining clean linens – Fresh towels and bed sheets minimize exposure to oil and acne-causing bacteria.
Consistently following these steps supports long-term back skin health and reduces the likelihood of persistent or severe bacne.
Treating Back Acne: Effective Strategies
Managing back acne starts with basic hygiene, especially for those who sweat frequently or are active outdoors. Oil, sweat, and dirt left on the skin can worsen pore blockages and inflammation.
Over-the-counter products are often the first line of treatment. Many cleansers, gels, and lotions contain active ingredients such as:
- Benzoyl peroxide – Reduces acne-causing bacteria and inflammation.
- Salicylic acid – Helps unclog pores by removing excess oil and dead skin cells.
- Alpha-hydroxy acids (AHAs) – Such as glycolic acid, which support gentle exfoliation.
Dr. Hannah Kopelman notes that low-to-medium concentrations of benzoyl peroxide are typically sufficient for the back, while higher levels may irritate sensitive skin. Salicylic acid provides a gentler alternative, and topical retinoids can be applied broadly rather than spot treatment. Products like Stridex pads can simplify daily care.
For severe or persistent bacne, medical consultation is recommended. Prescription treatments, clinical procedures, or combination therapies are often necessary, as back acne tends to be more stubborn and requires consistent, long-term management.
Back Acne vs. Other Body Acne: Key Differences
Although often grouped together, back acne differs from acne on other body areas in several ways. Skin structure, sebaceous gland density, and local triggers make bacne unique.
All body acne originates from clogged pores caused by sebum and dead skin cells. However, the back has thicker skin and larger sebaceous glands, so lesions are typically deeper, more inflamed, and harder to treat than acne on the chest, arms, or buttocks.
Key differences include:
- Location and skin thickness – The back is thicker; chest and shoulders are more sensitive.
- Inflammation levels – Bacne often appears as painful nodules or cysts.
- Specific triggers – Bacne is commonly caused by sweat and friction, while other body acne may relate more to products or hormonal changes.
- Treatment response – Back acne usually requires longer, more consistent care.
Understanding these distinctions helps guide realistic and targeted treatment strategies for each area of the body.
Best Ingredients for Treating Back Acne
Choosing the right active ingredients is crucial for effectively treating back acne. Because back skin is thicker and pores are larger, treatments need to penetrate deeply without causing excessive irritation.
Key ingredients for bacne include:
- Benzoyl peroxide – Reduces acne-causing bacteria and inflammation. Ideal for inflamed back acne, but should be introduced gradually to minimize irritation.
- Salicylic acid – Helps unclog pores by removing excess oil and dead skin cells; effective for blackheads and mild-to-moderate bacne.
- Retinoids – Promote cell turnover and prevent new pore blockages; usually applied broadly rather than as spot treatment.
- Alpha-hydroxy acids (AHAs) like glycolic acid – Provide gentle chemical exfoliation and improve skin texture.
- Niacinamide and sulfur – Soothe inflammation, regulate oil, and are suitable for sensitive skin.
A consistent regimen combining the right ingredients typically delivers the best results, helping reduce breakouts, calm inflammation, and improve overall back skin health.
How Long Does Back Acne Take to Clear?
A common question about bacne is how long it takes to improve. The answer varies depending on severity, causes, and treatment consistency.
For mild bacne, noticeable improvement usually occurs within 4–6 weeks when proper skincare and daily habits are maintained. Moderate to inflamed back acne may take 8–12 weeks, as back skin is thicker and cell turnover is slower than facial skin.
Cystic or chronic bacne often requires a longer duration and specialized medical treatment. Dermatologists may recommend combination therapy, including prescription topicals, oral medications, or clinical procedures.
Setting realistic expectations is essential. Bacne rarely clears instantly, and stopping treatment prematurely can slow results. Consistency, patience, and tailored care are key to achieving sustained improvement.
Common Mistakes That Make Back Acne Worse
Many daily habits, even with good intentions, can unintentionally worsen back acne. Recognizing these common mistakes helps ensure your skincare efforts are effective rather than counterproductive.
Frequent errors include:
- Over-cleansing or scrubbing too hard – Aggressive washing can damage the skin’s protective barrier and trigger inflammation.
- Delaying showers after sweating – Sweat left on the skin mixes with oil and bacteria, increasing pore blockages.
- Using comedogenic products – Haircare or body products that clog pores can worsen breakouts.
- Wearing tight clothing for long periods – Friction and pressure from clothes or sports gear can cause mechanical acne.
- Inconsistent skincare routine – Frequently switching products prevents skin from adjusting and slows improvement.
Avoiding these mistakes creates a healthier skin environment, enhancing the effectiveness of bacne treatment and supporting long-term back skin health.
Can Diet Really Affect Back Acne?
The link between diet and back acne remains debated, but increasing clinical evidence suggests certain foods may influence acne in some individuals. While diet isn’t the sole cause of bacne, nutrition can act as a trigger or worsen inflammation.
Foods commonly associated with back acne include:
- High-glycemic and sugary foods – Excess sugar spikes insulin, potentially boosting sebum production and inflammation.
- Dairy products – For some people, especially skim milk, dairy may affect hormones linked to acne.
- Low-fiber, low-antioxidant diets – Lack of skin-supporting nutrients can slow natural skin recovery.
Conversely, a balanced diet rich in vegetables, fruits, quality protein, and healthy fats can support overall skin function. Individual responses vary, so observing your skin’s reaction to dietary changes is often more effective than extreme restrictions.
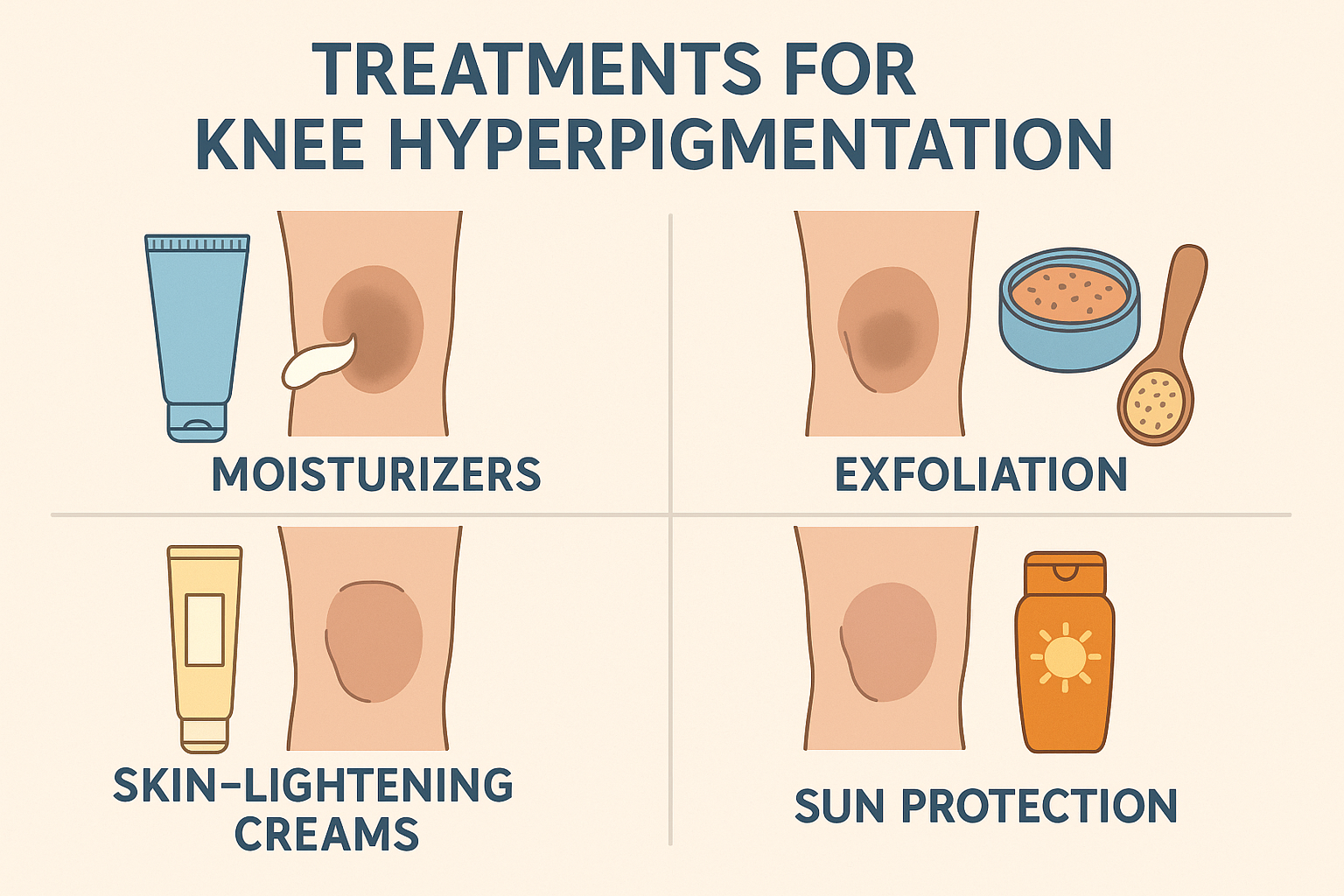
How to Prevent Bacne Scars and Dark Spots
Back acne can leave dark spots and scars, which are often harder to treat than active pimples. Early prevention is the most effective way to maintain even skin tone and texture.
Key strategies include:
- Control inflammation early – The longer acne is inflamed, the higher the risk of post-inflammatory hyperpigmentation and scarring. Consistent treatment reduces this risk.
- Avoid picking or scratching – Touching or squeezing acne damages skin tissue and worsens dark spots.
- Use skin-regenerating active ingredients – Retinoids, azelaic acid, niacinamide, and AHAs like glycolic acid help accelerate cell turnover and fade marks.
- Protect from sun exposure – UV rays can darken existing spots, making them more persistent.
For stubborn scars, clinical procedures like chemical peels or laser therapy may be recommended. Preventing marks from the start leads to better long-term results and smoother back skin.
Final Thoughts
Back acne is a common yet often overlooked skin condition that requires understanding and consistent care. Bacne develops from excess oil, clogged pores, bacteria, and lifestyle factors such as sweat, friction, hormones, and diet. Because back skin is thicker, lesions tend to be more inflamed and take longer to heal than facial acne.
Prevention through good hygiene, non-comedogenic products, and simple lifestyle adjustments reduces recurrence risk. Choosing appropriate active ingredients and using them consistently is crucial for healing, while avoiding common mistakes and addressing inflammation early helps prevent scars.
With the right approach and realistic expectations, back acne can be effectively managed, resulting in healthier, clearer skin over time.






 Acne
Acne Anti-Aging
Anti-Aging Business
Business Digital Marketing
Digital Marketing Economics
Economics Exfoliation
Exfoliation Hair Removal
Hair Removal Movies
Movies Personal Finance
Personal Finance Websites
Websites