8 Best Acne Treatments Recommended by Dermatologists for Effective Results

Acne is a very common skin condition that occurs when hair follicles beneath the skin become clogged with sebum (the skin’s natural oil) and dead skin cells. This blockage creates an ideal environment for the growth of Cutibacterium acnes bacteria, leading to inflammation, redness, and the formation of blackheads, whiteheads, pimples, or even cysts. Although acne affects up to 85% of people aged 12 to 24, it does not mean it should be left untreated — effective acne treatments are available to help manage and reduce symptoms.
Modern dermatology offers a wide range of scientifically proven acne treatments. Over-the-counter (OTC) products typically contain active ingredients such as benzoyl peroxide, salicylic acid, and retinoids. These help to unclog pores, reduce bacterial growth, and speed up skin cell turnover. For more severe cases, dermatologists may prescribe topical treatments, oral antibiotics, hormonal therapy, or isotretinoin.
Board-certified dermatologists—Dr Melanie Palm, Dr Sonia Batra, and Dr Brendan Camp—emphasise the importance of a personalised treatment approach. Factors like the type of acne (inflammatory, comedonal, or cystic) and skin sensitivity should be considered when selecting the most suitable therapy.
Types of Acne: Recognising and Understanding the Characteristics Before Starting Treatment
Before choosing the right acne treatment, it is essential to understand the type of acne you are dealing with. Each type has different causes, features, and treatment approaches.
- Comedonal Acne
Comedonal acne is the mildest form of acne, characterised by whiteheads and blackheads. It is caused by clogged pores due to a build-up of oil and dead skin cells. Dr Sonia Batra explains that comedones can develop from poor skin cell turnover or the use of heavy skincare and cosmetic products that block the pores.
- Inflammatory Acne
Inflammatory acne results from a combination of clogged pores and the overgrowth of bacteria on the skin, particularly Cutibacterium acnes. This type of acne appears as red bumps, papules, pustules, or even cysts. According to Dr Batra, excessive oil build-up can cause the walls of clogged pores to rupture beneath the skin, triggering the body’s inflammatory response.
- Cystic Acne
Cystic acne is a more severe form of inflammatory acne. It causes large, deep, and painful lesions beneath the skin. Dr Batra notes that this type is mainly driven by genetic factors, hormonal fluctuations, and more aggressive bacterial infections. If left untreated, cystic acne carries a high risk of permanent scarring.
- Hormonal Acne
Hormonal acne is triggered by hormonal changes, commonly occurring during menstruation, pregnancy, or menopause. It typically appears around the chin, jawline, and lower face. Most often affecting individuals aged 20 to 50, this type tends to present as cysts or inflamed bumps.1Hormonal acne: what is it, treatment, causes & prevention. Cleveland Clinic.
Understanding the characteristics of each acne type helps guide a more effective treatment strategy, tailored to your skin’s specific needs.
Here’s How Dermatologists Recommend Treating Acne
Gentle Cleanser
- Format: Over-the-Counter (OTC) Topical Treatments
- Acne Types Treated: Suitable for most types of acne, including comedonal acne, mild inflammatory acne, and mild hormonal acne.
Explanation: Using a gentle cleanser is a fundamental step in any acne skincare routine. According to Dr Sonia Batra, washing the face with a non-irritating cleanser helps remove excess oil (sebum), dirt, pollution, and cosmetic residue that can clog pores. Since clogged pores are the starting point for acne development, maintaining clean skin is a key preventive measure.
Gentle cleansers are formulated to clean the skin without disrupting its natural protective barrier or causing further irritation—both of which can worsen acne. These cleansers are typically free from harsh alcohols, fragrances, and abrasive ingredients that might trigger increased oil production or inflammation.
Dermatologists recommend using a gentle cleanser twice daily, in the morning and evening, as part of a regular skincare regimen to effectively manage acne. This step also helps prepare the skin to better absorb topical treatments such as benzoyl peroxide, retinoids, or antibiotics.
Benzoly Peroxide
- Format: Topical Medications (Available Over-the-Counter and by Prescription)
- Acne Types Treated: Inflammatory acne (such as papules and pustules) and non-inflammatory acne (such as blackheads and whiteheads)
Explanation: Benzoyl peroxide is one of the most widely used active ingredients in acne treatment. Commonly found in facial cleansers and spot treatments, it works through three main mechanisms: antibacterial, anti-inflammatory, and keratolytic (helping to shed dead skin cells).
According to Dr Brendan Camp, benzoyl peroxide is effective in killing Cutibacterium acnes—the bacteria involved in acne formation. It also helps prevent clogged pores by speeding up the removal of dead skin cells, while calming inflammation in already irritated skin.
However, Dr Melanie Palm cautions that benzoyl peroxide may cause side effects such as irritation, redness, or dryness, especially when applied to damp skin. To minimise these effects, it’s recommended to apply the product only after the face is fully dry and to start with a low concentration (2.5% to 5%), gradually increasing as needed.
When used consistently as part of a skincare routine, benzoyl peroxide can be highly effective in controlling and preventing new acne breakouts.
Salicylic Acid
- Format: Over-the-Counter (OTC) and Prescription Topical Treatments
- Acne Types Treated: Most effective for comedonal acne, including whiteheads and blackheads
Explanation: Salicylic acid is a key active ingredient in treating acne, especially comedonal acne. According to Dr Brendan Camp, it can be found in a variety of skincare products, including facial cleansers, toners, spot treatments, acne patches, and even some cosmetic products.
As a beta-hydroxy acid (BHA), salicylic acid has the unique ability to dissolve in oil, allowing it to penetrate deep into the pores. Once inside, it helps break down excess oil, dirt, and dead skin cells—the main culprits behind clogged pores and comedone formation.
Dr Melanie Palm notes that salicylic acid is an ideal alternative for individuals with sensitive skin who may not tolerate benzoyl peroxide well. With its gentler exfoliating action, it promotes skin cell turnover without causing excessive irritation.
When used consistently, salicylic acid can help prevent new breakouts, smooth skin texture, and keep pores clear and healthy.
Retinoids
- Format: Topical Medications (Available Over-the-Counter and by Prescription)
- Acne Types Treated: Effective for all types of acne, including inflammatory, cystic, and hormonal acne
Explanation: Retinoids are compounds derived from vitamin A and have long been considered the gold standard in acne treatment. Dr Sonia Batra explains that retinoids work by shrinking sebaceous glands (which produce oil), clearing clogged pores, and speeding up skin cell turnover, which helps prevent new acne breakouts.
Retinoid products come in different strengths:
- OTC (Over-the-counter) products like adapalene 0.1% are suitable for mild to moderate cases of acne.
- Prescription products, such as tretinoin or tazarotene, are used for more severe acne cases.
According to Dr. Batra, prescription-strength retinoids not only effectively reduce inflammation and prevent clogged pores but also help block the effects of androgen hormones that trigger excess oil production. Additionally, they have mild antibacterial properties.
However, retinoids can cause side effects like dry skin, redness, and peeling, especially in the early stages of use. Dr. Brendan Camp recommends starting with gradual application—such as 2–3 times a week—to build skin tolerance. Since retinoids increase sensitivity to UV rays, they should be used at night, and it’s essential to apply a moisturizer with SPF during the day to protect the skin.
Chemical Peels
- Format: Chemical Exfoliation Treatments (Available Over-the-Counter and by Prescription)
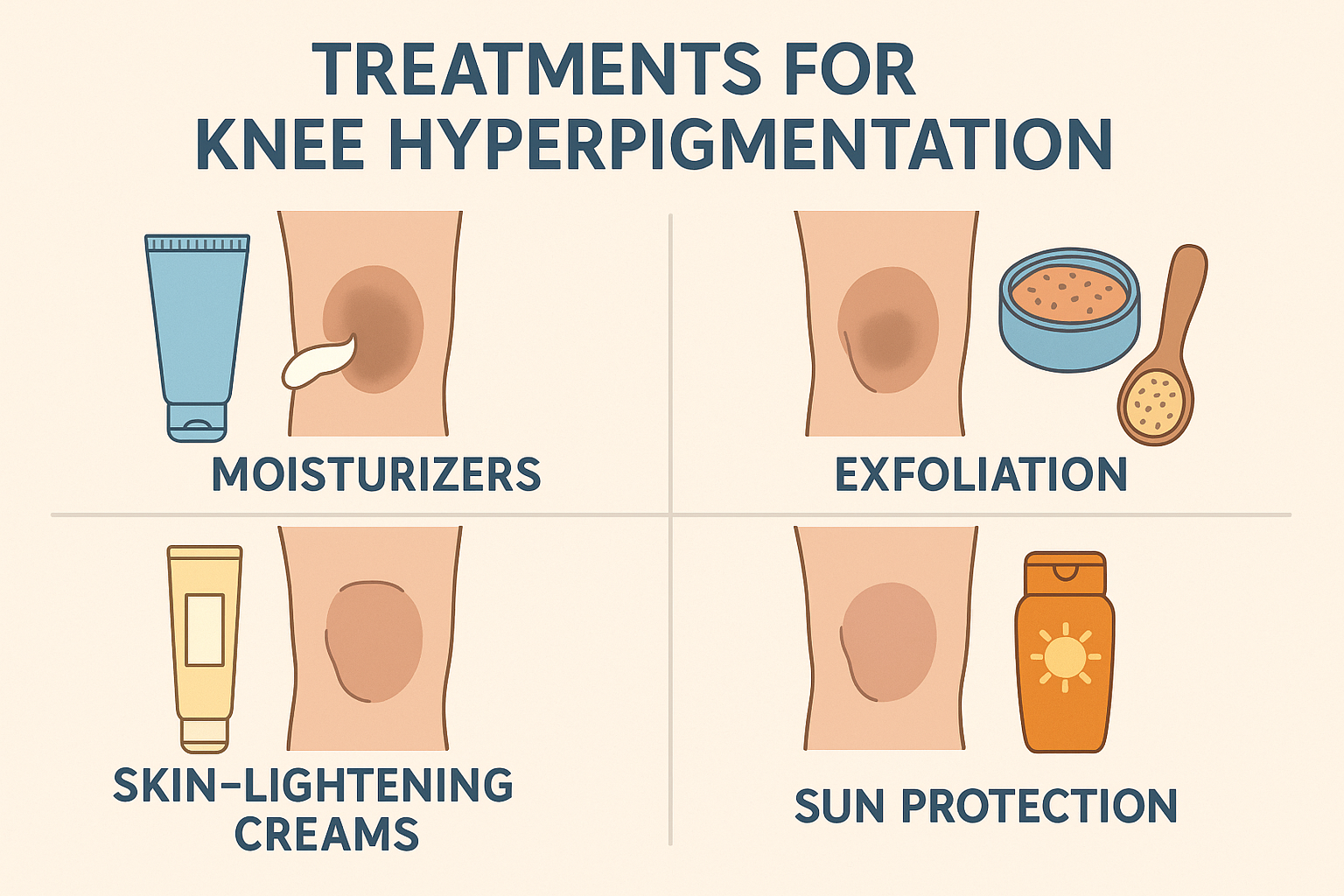
- Acne Types Treated: Various types of acne, including active acne, acne scars, and post-inflammatory hyperpigmentation
Explanation: Chemical peels are dermatological procedures designed to accelerate skin regeneration by exfoliating the damaged outer layers of the skin. According to Dr Sonia Batra, chemical peels work by speeding up cell turnover and helping to eliminate acne scars. These treatments often contain powerful exfoliants such as glycolic acid, salicylic acid, and lactic acid, each of which helps to clear clogged pores, reduce excess oil, and improve skin texture.
Dr. Melanie Palm explains that chemical peels performed in a dermatologist’s office can provide much more effective results than OTC products. In addition to treating active acne, these procedures also help reduce scarring and even out skin tone, particularly in cases of post-inflammatory hyperpigmentation. After the procedure, patients typically experience peeling for 5–7 days as part of the healing process.
However, it’s important to note that chemical peels are not recommended during pregnancy, as some of the active ingredients used may pose risks to the fetus.
With the right care and by choosing the appropriate type of peel, chemical peels can be an effective solution for improving acne-prone skin and accelerating the recovery of healthy skin.
Oral Antibiotics
- Format: Oral Prescription Medications (Taken by Mouth)
- Acne Types Treated: Moderate to severe inflammatory acne, including cystic acne
Explanation: Oral antibiotics are a primary treatment option for moderate to severe inflammatory and cystic acne. According to Dr. Brendan Camp, antibiotics like doxycycline, minocycline, and sarecycline work by inhibiting the growth of Cutibacterium acnes bacteria, which play a significant role in the inflammatory process of acne. In addition to their antibacterial properties, some antibiotics, like doxycycline, also have anti-inflammatory effects that help reduce redness and swelling on the skin.
Oral antibiotic therapy is typically prescribed for a limited period, usually between 1 to 3 months, to control active infection and inflammation. Long-term use is avoided to reduce the risk of antibiotic resistance.
In clinical practice, oral antibiotics are almost always combined with topical treatments like retinoids or benzoyl peroxide. This combination approach not only enhances the effectiveness of the treatment but also helps prevent bacterial resistance while speeding up skin healing. After completing antibiotic therapy, topical treatments are often continued to maintain results and prevent acne relapse.
It is essential to follow the prescribed duration and dosage of antibiotics carefully to achieve the best results and maintain long-term skin health.
Isotretinoin
- Format: Oral Prescription Medications
- Acne Types Treated: Severe cystic acne and inflammatory acne that does not respond to other treatments
Explanation: Isotretinoin, commonly known by the brand name Accutane, is one of the most effective prescription medications for treating severe acne. It is typically recommended by dermatologists for patients who have not seen improvements after trying various over-the-counter acne solutions or other topical treatments.2Pile HD, Sadiq NM. Isotretinoin. In: StatPearls. StatPearls Publishing; 2023.
According to Dr. Sonia Batra, isotretinoin works by shrinking the sebaceous glands, significantly reducing oil production. Additionally, isotretinoin helps reduce inflammation and prevents scarring, which are two critical factors in the treatment of cystic acne. By targeting the root causes of acne, isotretinoin remains one of the most important treatments available today.
Typically, isotretinoin therapy lasts between four to six months and requires strict medical supervision. Patients are required to have regular check-ups because isotretinoin can cause serious side effects, including dry skin, mood changes, and the risk of birth defects if used during pregnancy.
Although it requires close monitoring, isotretinoin is still considered a safe acne treatment for all skin types when used under proper medical supervision. This makes it a top choice in dermatologist-recommended treatments for severe cystic acne.
Spironolactone
- Format: Oral Prescription Medications
- Acne Types Treated: Hormonal acne in adult women
Explanation: Spironolactone is a prescription medication used to treat persistent hormonal acne, especially in adult women. Initially developed as a treatment for hypertension and heart conditions, spironolactone is now recognized as part of dermatologist-recommended acne treatments for skin conditions triggered by hormonal imbalances.
According to Dr. Murphy-Rose, spironolactone works as an androgen receptor antagonist, blocking the effects of androgen hormones, which play a role in increasing oil production in the skin. By inhibiting the interaction between androgen hormones and their receptors, spironolactone helps reduce excess oil, control acne, minimize hair loss, and prevent excessive hair growth on the face.
Most patients report good tolerance to spironolactone. However, like all systemic therapies, it can have potential side effects, including dizziness, nausea, dehydration, and menstrual irregularities. Therefore, regular monitoring by a doctor is necessary to ensure the treatment is safe and effective.
For individuals with acne-prone skin caused by hormonal fluctuations, spironolactone is considered one of the best acne treatments, safe and effective for all skin types when used at the proper dosage.
Conclusion
No matter what type of acne you have—ranging from mild comedonal acne to severe cystic acne—there are various treatment options available that can be tailored to your skin’s needs. From over-the-counter acne solutions like active ingredient-based cleansers to prescription acne medications such as retinoids and oral antibiotics, you have many ways to manage and treat your acne.
While over-the-counter products often serve as the first step in a skincare routine for acne-prone skin, successfully treating acne often requires professional intervention. How to treat acne professionally involves consulting with a licensed dermatologist who can accurately diagnose the type of acne and recommend the most appropriate therapy, including dermatologist-recommended acne treatments.
Dermatological consultation is particularly important if:
- Over-the-counter products are not providing sufficient results,
- Acne causes scarring or pigmentation changes,
- Acne negatively impacts your mental health or quality of life.
With the right medical approach, you can design a personalized skincare strategy, use the best ingredients for acne treatment, and ensure the therapies you choose are part of safe acne treatments for all skin types.
Don’t let acne go untreated. Seeking professional help can be a significant step toward clearer, healthier skin and greater confidence.
FAQ
In 2025, dermatologists consistently recommend a combination of benzoyl peroxide, retinoids (like adapalene), and salicylic acid-based products for treating mild to moderate acne. For persistent or severe cases, oral treatments such as antibiotics, hormonal therapy, or isotretinoin are carefully prescribed. Personalized treatment plans, supported by AI skin diagnostics, are also gaining traction for more targeted results.
Yes. Fast-acting acne treatments that deliver visible results often include topical benzoyl peroxide, light therapy (such as blue LED), and medical-grade skincare routines. However, the most effective results come from consistency, dermatologist guidance, and avoiding overuse of harsh products that damage the skin barrier.
Absolutely. Many mild to moderate acne cases respond well to non-prescription, science-backed skincare routines. Look for products with salicylic acid, niacinamide, or tea tree oil. Pair them with a consistent regimen, stress management, and a balanced diet. Still, for stubborn acne, a consultation with a board-certified dermatologist is the most effective path forward.






 Acne
Acne Anti-Aging
Anti-Aging Business
Business Digital Marketing
Digital Marketing Economics
Economics Exfoliation
Exfoliation Hair Removal
Hair Removal Movies
Movies Personal Finance
Personal Finance Websites
Websites