Melasma vs Hyperpigmentation: What a Dermatologist Says

If you’ve noticed dark patches on your skin, you might be dealing with melasma, hyperpigmentation, or even both. Think of it like squares and rectangles—melasma is a specific type of hyperpigmentation, but not all hyperpigmentation is melasma.[1Cleveland Clinic. Melasma]
Melasma often shows up as symmetrical brown patches on the face, particularly in women of reproductive age. It’s usually triggered by hormones, sun exposure, and genetics. In contrast, hyperpigmentation is a broader term that includes darkening caused by inflammation (like acne or eczema) or long-term UV exposure.
In this article, we’ll help you understand the key differences between melasma and other types of hyperpigmentation. By recognizing the signs and triggers, you’ll be better equipped to choose the right skincare treatment and prevent further skin discoloration.
Types of Hyperpigmentation and How to Recognize Them
Hyperpigmentation refers to areas of skin that appear darker than your natural tone, caused by an overproduction of melanin. There are three main types, each with distinct triggers and characteristics.
- Primary Pigment Disorders
These occur without any prior skin damage or inflammation. Similar to how some people are prone to acne or eczema, others naturally develop pigment changes. Melasma is one of the most common examples, especially affecting women and presenting as brown, symmetrical patches on the face.[2Plensdorf S, Livieratos M, Dada N. Pigmentation disorders: diagnosis and management. Am Fam Physician. 2017;96(12):797-804.] - Post-Inflammatory Hyperpigmentation (PIH)
PIH follows inflammation—think acne scars, eczema flare-ups, or even cuts. This type is more frequent in people with darker skin tones and often fades over time but can persist for weeks or months.[3Kaufman BP, Aman T, Alexis AF. Postinflammatory hyperpigmentation: epidemiology, clinical presentation, pathogenesis and treatment. Am J Clin Dermatol. 2018;19(4):489-503. doi:10.1007/s40257-017-0333-6.] - Sun-Induced Hyperpigmentation
This develops gradually due to chronic sun exposure. Besides wrinkles, UV rays can trigger sunspots and uneven pigmentation that dull the overall skin tone.
Understanding which type you have is key to choosing the right treatment and avoiding ineffective solutions.
What Is Melasma?
Melasma is a common pigment disorder marked by brown to dark brown patches on the face—especially on the forehead, cheeks, and upper lip.[4Cleveland Clinic: Melasma] These patches are symmetrical, appear slowly, and aren’t painful, itchy, or raised. There’s no flaking or acne-like texture—just a smooth change in skin color.
Hormonal changes are a major trigger. That’s why melasma often affects pregnant women or those using hormonal birth control.[5Key Derm Partners: Melasma vs. Hyperpigmentation] However, it can also appear in men or those without hormonal imbalances. People with medium to dark skin tones—such as those of Asian, Hispanic, or African descent—are more prone to developing melasma.[6Dr. Michele Green, MD: Best Melasma Treatment]
Sun exposure is the top aggravator. Symptoms often worsen in summer or with frequent time spent outdoors. Even visible light from screens and pollution can make melasma worse. That’s why sun protection is non-negotiable for managing this condition.
Melasma vs. Other Types of Hyperpigmentation: Key Differences
To tell melasma apart from other types of hyperpigmentation, focus on the cause and appearance. Melasma usually arises without any prior skin irritation and forms symmetrical patches, especially on the face. On the other hand, PIH follows inflammation—like acne or eczema—and may include signs like itchiness or leftover bumps.
Sun-induced hyperpigmentation and melasma both form without inflammation, but they behave differently. Melasma tends to follow a seasonal cycle—worsening in summer and improving in cooler months.[7Handel AC, Miot LD, Miot HA. Melasma: a clinical and epidemiological review. An Bras Dermatol. 2014;89(5):771-782. doi:10.1590/abd1806-4841.20143063.] In contrast, sunspots build up gradually over time from ongoing UV damage.
It’s also possible to experience multiple types at once. For example, you could have melasma from hormones, PIH from past acne, and sunspots from UV exposure. Skin tone plays a role too: PIH is more common in darker skin, while sun-induced pigmentation is more prevalent in lighter skin tones.[8Davis EC, Callender VD. Postinflammatory hyperpigmentation: a review of the epidemiology, clinical features, and treatment options in skin of color. J Clin Aesthet Dermatol. 2010;3(7):20-31.]
Proper diagnosis is essential for effective treatment. Misidentifying your condition could delay results and worsen pigmentation.
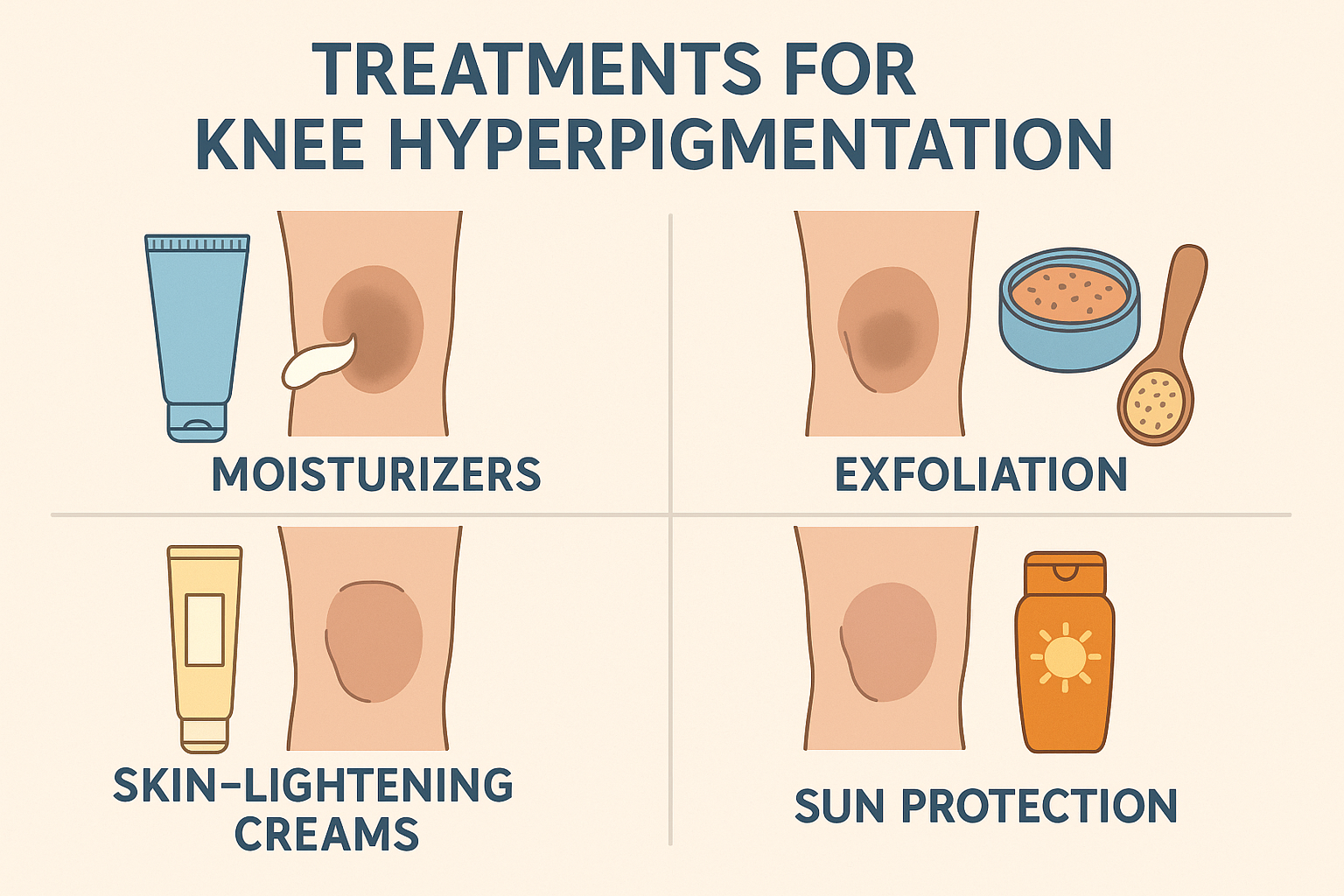
How to Treat Sun-Induced Hyperpigmentation Effectively
Sun-related pigmentation is one of the most preventable skin issues—making prevention your best strategy. Long-term exposure to UV rays is the root cause, so daily sun protection is essential.
1. Prevention Tips That Actually Work
Apply a broad-spectrum sunscreen every morning, regardless of the weather or whether you’re indoors. UV rays can penetrate windows and still affect your skin. Choose SPF 30 or higher, and reapply every two hours when outside.
For extra protection, wear wide-brimmed hats, UV-blocking sunglasses, and avoid direct sun during peak hours (10 a.m. to 4 p.m.). These habits don’t just prevent hyperpigmentation—they also slow down skin aging and reduce your risk of skin cancer.
If you already have melasma or PIH, sun protection is still crucial. UV exposure can worsen these conditions, making treatment slower and less effective. In short, sunscreen isn’t optional—it’s your skin’s daily armor.
2. Best Topical Ingredients for Sun-Induced Hyperpigmentation
Topical antioxidants like vitamin C and vitamin E are powerful tools in fading sun-induced dark spots. These ingredients work by neutralizing free radicals and slowing down melanin overproduction. In addition, retinol boosts cell turnover, helping your skin shed pigmented cells and reveal a more even tone over time.[9Davis EC, Callender VD. Postinflammatory hyperpigmentation: a review of the epidemiology, clinical features, and treatment options in skin of color. J Clin Aesthet Dermatol. 2010;3(7):20-31.]
Used consistently, this combination not only fades existing discoloration but also prevents new pigmentation from forming. For best results, apply these products at night and always follow up with sunscreen in the morning. This protects your skin from further UV damage and prevents irritation caused by active ingredients.
Consistency is key—topicals work gradually, but with daily use, they can significantly improve skin clarity and brightness.
3. Chemical Peels: A Powerful Option for Pigmentation
Chemical peels are an effective treatment for sun-related hyperpigmentation. These procedures remove the outer layer of dead skin using exfoliating acids like glycolic acid, lactic acid, salicylic acid, retinol, trichloroacetic acid (TCA), or hydroquinone.
Peels can be performed by dermatologists in a clinical setting or used at home in milder forms. Over time, the peeling process encourages the growth of new, brighter skin cells, reducing uneven pigmentation.
Visible results develop gradually with repeated sessions. However, post-peel care is crucial—always use sunscreen afterward to protect your newly sensitive skin and avoid rebound pigmentation.
4. Laser Treatments for Targeted Pigment Removal
Laser therapy is a high-tech option for treating sun-induced hyperpigmentation. Devices like Intense Pulsed Light (IPL) and Clear + Brilliant target diffuse redness and brown spots by breaking down melanin in the upper layers of the skin.[10Arora P, Sarkar R, Garg VK, Arya L. Lasers for treatment of melasma and post-inflammatory hyperpigmentation. J Cutan Aesthet Surg. 2012;5(2):93-103. doi:10.4103/0974-2077.99436.]
For deeper or more stubborn sunspots, lasers with 755-nm or 1064-nm wavelengths are used. These penetrate the skin more deeply to destroy pigment clusters without harming surrounding tissue.
While results can be dramatic, multiple sessions are often needed. Always choose a licensed professional for laser treatment, and follow strict sun protection guidelines afterward to preserve the results and avoid recurrence.
How to Treat Post-Inflammatory Hyperpigmentation (PIH)
1. Prevention Is the First Step
The most effective way to prevent post-inflammatory hyperpigmentation (PIH) is to control skin inflammation early. PIH often lasts longer than the original flare-up, so treating underlying conditions like acne, eczema, or skin infections quickly and thoroughly is essential.
This may involve topical corticosteroids, antibiotics, or even oral or injectable therapies for severe cases. The faster the inflammation is reduced, the lower the chance of excess pigment forming.
Avoid scratching, picking, or popping inflamed skin—this can worsen PIH by causing physical trauma. Once inflammation has subsided, consistent use of sunscreen is critical to prevent dark marks from becoming more pronounced due to UV exposure.
2. Topical Treatments for PIH: What Works
For acne-prone skin, topical treatments like retinol, azelaic acid, and vitamin C are effective for fading PIH. These ingredients help speed up cell turnover, reduce melanin production, and calm mild inflammation—leading to clearer skin over time.
However, those with eczema or sensitive skin need a more cautious approach. Many active ingredients for pigmentation can be irritating and may worsen delicate skin if used improperly.
In such cases, start with low concentrations and monitor your skin’s response carefully. Consulting a dermatologist before beginning treatment is highly recommended. A gentle, consistent routine is the key to improvement without triggering new flare-ups.
3. Chemical Peels for Treating PIH
Chemical peels can be an effective option for treating post-inflammatory hyperpigmentation (PIH), especially when done in a gradual and controlled manner. Ingredients like glycolic acid, lactic acid, salicylic acid, retinol, trichloroacetic acid (TCA), and hydroquinone help remove dead skin cells and stimulate the renewal of brighter, more even-toned skin.[11Rendon MI, Berson DS, Cohen JL, Roberts WE, Starker I, Wang B. Evidence and considerations in the application of chemical peels in skin disorders and aesthetic resurfacing. J Clin Aesthet Dermatol. 2010;3(7):32-43.]
Since PIH commonly affects darker or more sensitive skin, professional supervision is essential. Overusing strong ingredients or peeling too frequently may lead to irritation or worsen pigmentation.
For optimal results, the treatment plan should be customized based on your skin type and sensitivity. A step-by-step approach with regular monitoring is the safest and most effective way to fade PIH while avoiding setbacks.
4. Laser Treatments for PIH: Safe and Precise Options
Gentle laser technologies like picosecond or microsecond lasers can help reduce post-inflammatory hyperpigmentation safely. These treatments target excess melanin without damaging surrounding tissue, allowing dark marks to fade gradually.[12Arora P, Sarkar R, Garg VK, Arya L. Lasers for treatment of melasma and post-inflammatory hyperpigmentation. J Cutan Aesthet Surg. 2012;5(2):93-103. doi:10.4103/0974-2077.99436.]
Since PIH-prone skin is often sensitive, laser procedures must be performed by experienced professionals. Incorrect settings or technique may lead to burns, scarring, or new pigmentation issues.
A thorough skin evaluation—including tone, sensitivity, and history—is crucial before undergoing laser therapy. When done right, laser treatment can be a powerful tool in restoring even skin tone and improving overall complexion.
Melasma: Prevention and Treatment That Work
1. Daily Protection from Sun and Visible Light
Melasma is extremely sensitive to both UV and visible light, so consistent sun protection is non-negotiable. Use a broad-spectrum SPF 30+ sunscreen every day—rain or shine, indoors or out.
Tinted physical sunscreens containing zinc oxide or titanium dioxide are especially recommended. Their iron oxide pigments not only shield the skin from UV rays but also block visible light, including light from lamps and screens.
For added defense, Dermablend Flawless Creator foundation is a great option. It contains iron oxides that further protect against light-triggered melasma flares while evening out skin tone. Layering sunscreen and pigmented makeup gives your skin dual protection and boosts treatment results.
2. Hormone-Free Birth Control Alternatives
Since estrogen can trigger or worsen melasma, switching to estrogen-free birth control may help manage the condition. Options include progestin-only pills, hormonal IUDs (like levonorgestrel), or non-hormonal methods like condoms or diaphragms.
However, every contraceptive method has its own benefits and risks. It’s important to discuss these options with both your gynecologist and dermatologist to find a solution that supports your reproductive health without aggravating your melasma.
An integrated, personalized approach offers the best results for both skin and overall well-being.
3. Topical Skincare for Melasma
Topical treatments are essential for managing melasma. These products work by reducing melanin production and speeding up skin cell turnover. Common active ingredients include glycolic acid (exfoliation), vitamin C (antioxidant and brightening), and retinol (cell renewal).[13Ogbechie-Godec OA, Elbuluk N. Melasma: an up-to-date comprehensive review. Dermatol Ther (Heidelb). 2017;7(3):305-318. doi:10.1007/s13555-017-0194-1.]
Other effective agents include azelaic acid, kojic acid, and tranexamic acid, which inhibit tyrosinase—an enzyme involved in melanin production. Niacinamide also helps strengthen the skin barrier and gradually reduce pigmentation.
For stubborn melasma, dermatologists may prescribe hydroquinone, a powerful skin-lightening agent. However, hydroquinone must be used under strict medical supervision, as overuse can lead to irritation or worsening of pigmentation.
Consistency, correct ingredient choice, and sun protection are key to successful melasma treatment.
4. Oral Therapy for Melasma
In more severe or treatment-resistant melasma cases, oral tranexamic acid may be considered. This medication works by blocking plasminogen activation, reducing inflammation and pigment formation in the skin.
Studies show that oral tranexamic acid can effectively lighten melasma and prevent recurrences. However, it carries potential side effects such as digestive discomfort, headaches, and increased risk of blood clots.[14Bala HR, Lee S, Wong C, Pandya AG, Rodrigues M. Oral tranexamic acid for the treatment of melasma: a review. Dermatol Surg. 2018;44(6):814-825. doi:10.1097/DSS.0000000000001518.]
That’s why this therapy should only be taken under the guidance of a certified dermatologist who understands your medical history. A full discussion of benefits and risks is crucial before starting treatment to ensure both safety and effectiveness.
5. Chemical Peels for Melasma
Chemical peels help exfoliate dead skin cells and stimulate the growth of new, more evenly pigmented cells. For melasma, clinical or at-home peels often include glycolic acid, lactic acid, salicylic acid, retinol, TCA, or hydroquinone.[15Rendon MI, Berson DS, Cohen JL, Roberts WE, Starker I, Wang B. Evidence and considerations in the application of chemical peels in skin disorders and aesthetic resurfacing. J Clin Aesthet Dermatol. 2010;3(7):32-43.]
While effective, chemical peels for melasma must be approached with caution. Melasma-prone skin is sensitive, especially in darker skin tones. Aggressive peels or strong formulas can backfire, leading to inflammation and worsening pigmentation.
That’s why peels must be tailored to your skin type, with carefully selected ingredients, strengths, and frequency. A conservative, dermatologist-guided routine is key to getting visible results without setbacks.
6. Laser Treatments for Melasma: Effective, but With Caution
Low-energy laser therapy may help treat stubborn melasma, especially when topical treatments and peels aren’t enough. Devices like picosecond lasers or Q-switched Nd:YAG lasers target melanin selectively without damaging healthy skin.[16Arora P, Sarkar R, Garg VK, Arya L. Lasers for treatment of melasma and post-inflammatory hyperpigmentation. J Cutan Aesthet Surg. 2012;5(2):93-103. doi:10.4103/0974-2077.99436.]
However, melasma is highly reactive to light, and improper laser use can worsen the condition. That’s why it’s critical to have laser treatments done by an experienced dermatologist who understands your skin type and melasma severity.
A thorough evaluation, proper settings, and post-treatment sun protection are essential to ensure success and avoid relapse.
Conclusion: Understanding and Managing Skin Pigmentation
Melasma is just one form of hyperpigmentation—but not all hyperpigmentation is melasma. Think of melasma as a square within the larger category of hyperpigmentation (a rectangle). The three main types include primary pigment disorders (like melasma), post-inflammatory hyperpigmentation (PIH), and sun-induced pigmentation.
Each type has different causes and responds best to specific treatments. Regardless of the cause, a comprehensive approach—daily sun protection, targeted topical care, and cautious use of peels or lasers—forms the foundation of effective pigmentation management.
With the right knowledge and personalized treatment plan, you can restore a more even, radiant complexion—and keep it that way.
About the Author
M. Hariri is a business and beauty content writer with over five years of experience. He focuses on research-based skincare education and frequently collaborates with dermatologists. His work can be found in various national and international beauty publications.






 Acne
Acne Anti-Aging
Anti-Aging Business
Business Digital Marketing
Digital Marketing Economics
Economics Exfoliation
Exfoliation Hair Removal
Hair Removal Movies
Movies Personal Finance
Personal Finance Websites
Websites