Fungal Acne Treatment: 10 Steps Backed by Dermatologists

Not all breakouts are caused by clogged pores or hormonal shifts. Behind seemingly clear skin, a lesser-known condition may be lurking—fungal acne. Despite the name, it’s not a true acne but a yeast-related skin issue caused by an overgrowth of Malassezia fungi.
Unlike bacterial acne, fungal acne needs a different treatment approach. It often looks similar—tiny, uniform bumps that appear on the chest, back, or face—but it tends to feel itchy and doesn’t respond to typical acne products.
This article breaks down 10 dermatologist-backed steps to manage and treat fungal acne effectively. You’ll learn how to recognize the symptoms, prevent flare-ups, and apply the right treatments early on—without wasting time on methods that won’t work.
What Is Fungal Acne?
Fungal acne isn’t technically acne. It’s a form of folliculitis—an inflammation of the hair follicles—caused by an overgrowth of Malassezia yeast on the skin. The medical term is Malassezia folliculitis or Pityrosporum folliculitis.
This condition often flares in hot, humid environments or when sweat and oil build up, especially in tight clothes. You’ll likely see small, itchy bumps in clusters on the back,[1Cleveland Clinic: Acne. Updated September 1, 2020.] chest, shoulders, or even the forehead—often mistaken for whiteheads.
A key sign? Itchiness and uniform bumps. Unlike bacterial acne, fungal acne tends to appear all at once and doesn’t respond to common acne treatments. That’s why understanding the difference is crucial—misdiagnosis can delay effective treatment.
What Causes Fungal Acne? 4 Key Triggers You Should Know
Fungal acne happens when the natural balance of microbes on your skin shifts—especially in warm, sweaty conditions. Here’s what commonly triggers it:
- Heat & Humidity
Hot, tropical climates make your skin sweatier, creating a perfect environment for yeast overgrowth.[2Cohen PR, Erickson C, Calame A. Malassezia (pityrosporum) folliculitis incognito: malessezia-associated folliculitis masked by topical corticosteroid therapy. Cureus. 2020;12(1):e6531. doi:10.7759/cureus.6531] - Trapped Sweat
Wearing tight clothing or skipping a post-workout shower can trap sweat, feeding fungal growth in hair follicles—especially on the back and chest. - Overuse of Antibiotics
Long-term antibiotic use can kill off beneficial bacteria, allowing Malassezia yeast to thrive unchecked. - Skin-to-Skin Contact
Though not highly contagious, direct contact with someone who has fungal acne may spread the yeast, especially in shared environments.
Knowing these triggers helps you take preventive steps and avoid recurring flare-ups.
How to Prevent Fungal Acne
Prevention starts with keeping your skin cool, clean, and dry—especially if you live in a hot climate or sweat frequently. Dermatologists recommend wearing loose, breathable fabrics like cotton. Avoid tight synthetics like spandex that trap moisture.
After workouts or heavy sweating, change clothes immediately and shower as soon as possible to remove excess oil and sweat that feed fungal growth.
Review your antibiotic use as well—long-term use may disrupt your skin’s microbiome, making it easier for fungi to overgrow. If you’re noticing persistent breakouts while on antibiotics, speak with your doctor about adjusting your treatment.
Daily hygiene and smart skincare choices are your best defense against future fungal acne flare-ups.
What’s the Best Way to Treat Fungal Acne at Home?
Once you suspect your breakouts are fungal, the good news is that treatment can start right at home. Unlike typical acne, fungal acne responds best to antifungal ingredients—many of which are already available over-the-counter.
Dermatologists highlight that the condition is often easier to treat than other forms of acne—if you target the root cause. That means avoiding regular acne treatments that might actually worsen the issue.
Starting early with the right products can help clear your skin without a prescription—and prevent missteps that prolong the problem.
1. Use an Anti-Dandruff Shampoo as a Cleanser
A surprising but effective fix: anti-dandruff shampoo. Look for formulas with zinc pyrithione or ketoconazole—both are antifungal agents proven to combat Malassezia.
Though made for the scalp, these shampoos can be used as a body or facial cleanser wherever fungal acne appears. Apply a thin layer to the affected area, leave it on for about 1 minute, then rinse thoroughly. This contact time helps the active ingredients work effectively.
Use once or twice a day depending on the severity. This simple, accessible treatment is often the first—and most effective—step before turning to prescription solutions.
2. Apply a Topical Antifungal Cream
It may sound unconventional, but over-the-counter athlete’s foot creams can help treat fungal acne. Why? Both conditions are caused by similar types of Malassezia yeast. These creams typically contain antifungal agents like clotrimazole or miconazole that work by reducing yeast overgrowth on the skin.
Dermatologists often recommend these creams for mild to moderate cases of Malassezia folliculitis. Simply apply a thin layer to clean, dry skin twice a day.
If you don’t notice visible improvement within 1 to 2 weeks, consult a dermatologist. Persistent symptoms may signal a misdiagnosis or the need for stronger medication. Proper assessment ensures your treatment is accurate and effective.
3. Use Prescription Antifungal Creams If Needed
When OTC creams fail, it’s time to see a dermatologist. Prescription-strength topical antifungals—such as ketoconazole 2%—are often recommended for moderate to severe fungal acne.
These creams target the root cause by directly inhibiting fungal growth. Most dermatologists advise using them twice daily for about 2–3 weeks, though duration may vary based on severity and skin response.
According to Dr. Andrea Suarez (board-certified dermatologist), targeted antifungal therapy not only clears the infection faster but also lowers the risk of recurrence. Be sure to follow your doctor’s instructions carefully. If irritation or lack of improvement occurs, revisit your provider for a treatment adjustment.
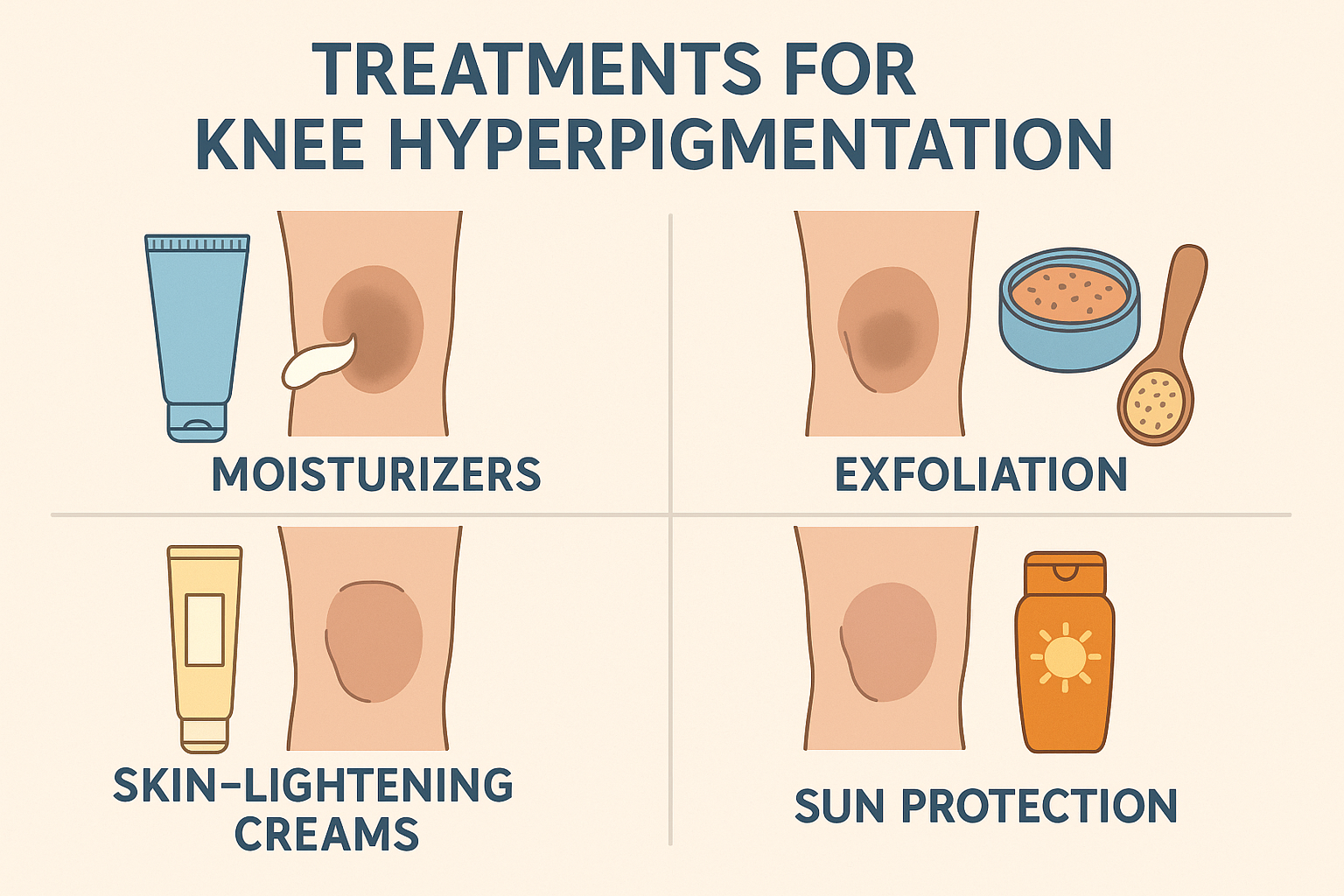
4. Exfoliate to Remove Oil and Dead Skin
Regular exfoliation is key to preventing fungal acne. Dead skin cells, excess oil, and sweat residue can trap moisture and feed fungal growth.[3Coleman J, Johnson SM. The importance of recognizing yeast acne malessezia versus propionbacterium. J Ark Med Soc. 2017;113(7):164-165.] Gentle exfoliation helps unclog pores and reduces this buildup—limiting the yeast’s food source.
Experts recommend using chemical exfoliants like salicylic acid or gluconolactone. These are gentle yet effective, especially after workouts or heavy sweating.
Limit exfoliating to 2–3 times a week to avoid over-stripping your skin. Overdoing it can damage your skin barrier and make fungal acne worse. Balanced exfoliation keeps your skin clean, smooth, and less prone to flare-ups.
5. Wipe Sweat Off with Acne-Friendly Body Wipes
Can’t shower right after working out? Use acne-safe wipes as a quick fix. Keeping your skin clean and dry after sweating is crucial to prevent fungal acne.
Choose wipes that contain salicylic acid to help dissolve oil and reduce clogged pores. This ingredient also has anti-inflammatory properties, making it suitable for sensitive, acne-prone skin.
Focus on sweat-prone areas like your back, chest, and underarms. While not a replacement for showering, these wipes are a great temporary solution—especially in hot, humid climates or during busy days.
Smart hygiene hacks like this help minimize moisture and keep fungal acne under control until you can wash up properly.
6. Choose an Oil-Free Moisturizer to Stay Hydrated
Hydration is important, even when dealing with fungal acne—but the right kind of moisturizer matters. Malassezia yeast thrives in oily environments, so opt for an oil-free, non-comedogenic formula.
After applying antifungal creams or exfoliants, your skin might feel dry or irritated. A lightweight, water-based moisturizer helps soothe and hydrate without feeding the fungus.
Look for ingredients like glycerin, hyaluronic acid, or panthenol. These attract moisture and calm the skin without leaving a greasy residue. Avoid thick, oil-rich products like coconut oil or shea butter, which can worsen fungal breakouts.
With the right moisturizer, you can support healing and maintain healthy skin—without compromising your fungal acne treatment.
7. Try Tea Tree Oil as a Natural Add-On
Tea tree oil is a popular natural remedy with antifungal and antiseptic properties, making it a useful complementary treatment for fungal acne. It helps inhibit the growth of Malassezia yeast on the skin.
However, it should never be applied directly. Dilute 1–2 drops of tea tree oil with about 12 drops of a carrier oil like jojoba or fractionated coconut oil. Then apply it to the affected area. Never ingest it.
Before full use, perform a patch test—especially if you have sensitive skin. If no redness, itching, or irritation appears within 24 hours, it’s likely safe to use topically. When used correctly, tea tree oil can gently support your antifungal skincare routine.
8. Use the Right Anti-Blemish Serum
A well-formulated anti-blemish serum can help speed up recovery and fade post-acne marks. Look for lightweight, oil-free serums that contain ingredients like niacinamide, salicylic acid, or azelaic acid. These help calm inflammation and brighten dark spots.
Since fungal acne worsens with heavy or oily products, choose non-comedogenic serums specifically made for acne-prone skin. Many advanced formulas treat active breakouts while reducing discoloration.
Apply your serum after cleansing and before moisturizing. With consistent use, it can enhance your results and prevent visible scarring—supporting a clearer, smoother complexion over time.
9. Take Oral Antifungal Medication When Needed
For stubborn or widespread fungal acne, oral antifungals like fluconazole may be prescribed by a dermatologist. These medications work systemically to reduce fungal growth from within the body.
In moderate to severe cases, oral treatment often delivers faster and more lasting results than topical options alone. It’s especially useful when the infection spreads beyond localized areas.
Since these drugs affect your whole system, they must be taken under medical supervision. Your doctor will determine the right dosage and duration based on your skin condition and health profile to maximize safety and effectiveness.
10. Wear Loose, Breathable Clothing
One of the easiest ways to prevent fungal acne is to wear breathable, loose-fitting clothing—especially in hot or humid conditions. Tight clothes made from synthetic fabrics like spandex trap heat and moisture, creating a perfect breeding ground for yeast.
According to dermatologists, this is a common trigger for fungal folliculitis, especially on the back, chest, and skin folds. Switch to natural fabrics like cotton or linen to allow better airflow and reduce skin irritation.
Always change out of sweaty clothes after exercise or intense heat exposure. These simple steps help keep your skin clean and dry, reducing the risk of future fungal breakouts—particularly for active individuals or those in tropical climates.
Best Over-the-Counter Products for Fungal Acne
For mild to moderate fungal acne, OTC antifungal products can be highly effective if used correctly. Dermatologists often recommend starting here before trying prescription options.
Look for active ingredients like ketoconazole, zinc pyrithione, or clotrimazole. Some trusted choices include:
- Nizoral Anti-Dandruff Shampoo (1% ketoconazole) – can double as a body or facial cleanser.
- Head & Shoulders Classic Clean (zinc pyrithione) – ideal for scalp or back acne.
- Canesten Cream (clotrimazole) – works well on isolated body areas.
- Selsun Blue Medicated (selenium sulfide) – another antifungal alternative.
Use as directed and be patient—it may take a few weeks to see improvement. If your condition doesn’t get better, consult a dermatologist for further guidance.
Skincare Ingredients to Avoid with Fungal Acne
The wrong skincare ingredients can worsen fungal acne by feeding Malassezia. Avoiding certain oils and emollients is crucial for recovery and prevention.
Experts advise steering clear of:
- Coconut oil
- Olive oil
- Shea butter
- Lanolin
- Fatty acid derivatives like esters and polysorbates
These ingredients can clog pores and promote fungal growth, especially in humid conditions. Also skip overly occlusive moisturizers that trap heat and moisture.
Instead, choose water-based, non-comedogenic, and oil-free skincare products. By avoiding fungal triggers in your routine, you support healing and reduce the chances of recurrence.






 Acne
Acne Anti-Aging
Anti-Aging Business
Business Digital Marketing
Digital Marketing Economics
Economics Exfoliation
Exfoliation Hair Removal
Hair Removal Movies
Movies Personal Finance
Personal Finance Websites
Websites