How to Use Nizoral for Acne: Dermatologists Explain

Not all acne is caused by stress, hormones, or bacteria. In some cases, the real culprit is a yeast overgrowth known as fungal acne (medically: pityrosporum folliculitis). This condition causes inflamed, itchy bumps that often mimic regular acne but require a very different approach.[1Cleveland Clinic. Acne. Updated September 1, 2020.]
Because it’s fungal—not bacterial—typical acne treatments don’t work and may even worsen the condition. That’s where Nizoral comes in. Originally formulated as an anti-dandruff shampoo, Nizoral contains ketoconazole, an antifungal agent shown to effectively target the root cause of fungal acne.
According to board-certified dermatologists, using Nizoral topically can help reduce inflammation and eliminate yeast buildup on the skin. If your acne doesn’t respond to standard products, you might be dealing with a fungal issue—and Nizoral could be the missing piece in your skincare routine.
Want to know how to use it safely and effectively? Keep reading for expert-backed tips and product recommendations.
What Is Nizoral and How Does It Work?
Nizoral is an over-the-counter antifungal treatment containing ketoconazole, a powerful ingredient that stops the growth of yeast on the skin.[2Cleveland Clinic: Ketoconazole Shampoo.] While commonly used to treat dandruff and seborrheic dermatitis, it’s also helpful in managing skin issues like fungal acne.
Ketoconazole works by disrupting the structure of fungal cell membranes, effectively stopping the fungi from multiplying. As the yeast dies off, inflammation, itchiness, and breakouts begin to subside.
Dermatologists now recognize Nizoral’s potential beyond scalp care. For stubborn acne that doesn’t clear with salicylic acid or benzoyl peroxide, Nizoral might be the solution—especially if it’s fungal in nature.
However, not all acne is fungal. If you’re unsure, consult a skin professional before adding Nizoral to your skincare routine. Understanding the type of acne you’re dealing with is key to effective treatment and long-term results.
Benefits of Nizoral for Fungal Acne and Skin Infections
Fungal acne often shows up as small, itchy bumps that don’t respond to regular acne treatments. The culprit? A yeast called Malassezia, the same microorganism responsible for dandruff. This yeast thrives in oily, humid environments and can affect your face, chest, back, and scalp.
Nizoral’s active ingredient, ketoconazole, effectively reduces yeast on the skin, making it a go-to solution for pityrosporum folliculitis. Though designed as a dandruff shampoo, Nizoral works well when used as a face and body wash in targeted areas.
Beyond fungal acne, Nizoral can also treat other fungal infections like athlete’s foot and ringworm. Its multi-use benefits make it a practical product to keep on hand, especially if you’re prone to skin issues triggered by excess oil or sweat.[3Michigan Medicine University of Michigan. Ketoconazole topical. Updated January 10, 2019.]
For best results, apply once or twice daily to clean, dry skin. Leaving it on for about 30 seconds before rinsing helps maximize its antifungal action.
Possible Side Effects of Using Nizoral
While Nizoral is generally safe for topical use, it’s not entirely risk-free. Mild side effects such as redness, dryness, or itching may occur, especially during the first few uses. These reactions are usually temporary and subside with continued use.
Serious side effects are rare when Nizoral is used externally. However, if you notice burning, worsening irritation, or signs of an allergic reaction, stop using it and consult a dermatologist.
The oral version of Nizoral—available only by prescription—has more significant risks, including nausea, liver issues, and hormonal imbalances. That’s why doctors recommend sticking to the topical form for skin-related fungal concerns unless directed otherwise.
Pregnant or breastfeeding? Always check with a healthcare provider first. Though topical absorption is minimal, it’s better to stay cautious, especially when using products on large skin areas or long-term.[4Cleveland Clinic. Ketoconazole tablets.]
How to Safely Use Nizoral for Acne-Prone Skin
Using Nizoral correctly is key to seeing results. For fungal acne, dermatologists recommend applying it once daily for the first two weeks, then reducing to twice a week for maintenance.
Although it’s labeled as a shampoo, Nizoral can be used like a facial cleanser. Apply a thin layer to the affected area, leave it on for 30 seconds, and rinse thoroughly. This contact time allows ketoconazole to work its antifungal magic.
You should start noticing improvements within two to four weeks. If not, consult a dermatologist to reassess your skin condition—it might not be fungal after all.
To boost results, combine Nizoral with non-comedogenic skincare. Ingredients like salicylic acid pair well with Nizoral, but avoid oils like coconut oil, which can feed yeast. Keep your skin dry and clean, especially in hot, humid climates where fungal acne tends to thrive.
Nizoral vs. Regular Acne Cleansers: Which One Is Better?
Most popular acne cleansers—like CeraVe Renewing SA Cleanser—are designed to treat common acne caused by excess oil, clogged pores, and bacteria. They often contain ingredients like salicylic acid, which helps exfoliate dead skin cells and reduce inflammation.
However, these cleansers don’t address fungal acne. While salicylic acid may help control oil and support skin turnover, it doesn’t eliminate Malassezia, the yeast responsible for fungal breakouts.
That’s where Nizoral stands out. Its active ingredient, ketoconazole, directly targets the root cause—fungal overgrowth—not just surface symptoms. If your acne isn’t improving with traditional face washes, it may be time to try an antifungal approach.
Choosing the right product isn’t about trends—it’s about understanding what’s really causing your skin issues. If your breakouts are itchy, uniform, or resistant to regular treatment, Nizoral may be the game-changer your skin needs.
How to Tell the Difference Between Fungal and Bacterial Acne
Fungal and bacterial acne can look similar—but they’re very different conditions. Bacterial acne is often caused by clogged pores, oil, and bacteria. It ranges from blackheads to painful pustules and usually responds to salicylic acid or benzoyl peroxide.
Fungal acne, or Malassezia folliculitis, is caused by yeast overgrowth inside hair follicles. It often appears as small, itchy bumps that cluster on oily or humid areas like the forehead, chest, or back.
A quick way to tell the difference? Pay attention to treatment results. If your acne doesn’t improve after using regular acne products for weeks, it could be fungal—and you may benefit more from antifungal treatments like Nizoral.
Knowing what type of acne you’re dealing with is key to clearing your skin and avoiding unnecessary irritation from the wrong products.
Who’s Most at Risk of Developing Fungal Acne?
Fungal acne can affect anyone, but it’s more common among certain groups. If you have oily skin, sweat frequently, or live in a hot, humid climate, you may be more prone to it.
Wearing tight clothing or helmets for long periods can trap moisture and heat—perfect conditions for fungal growth. Athletes and physically active individuals are especially at risk if they don’t shower or change clothes soon after sweating.
Long-term antibiotic use can also disrupt the skin’s natural balance, allowing yeast to overgrow. Similarly, using oil-heavy skincare products—like coconut or olive oil—can feed the fungus and worsen breakouts.
If you check one or more of these boxes, pay close attention to persistent acne that doesn’t respond to standard treatments. A simple switch to antifungal care could make all the difference.
Safe Skincare Ingredients to Pair with Nizoral
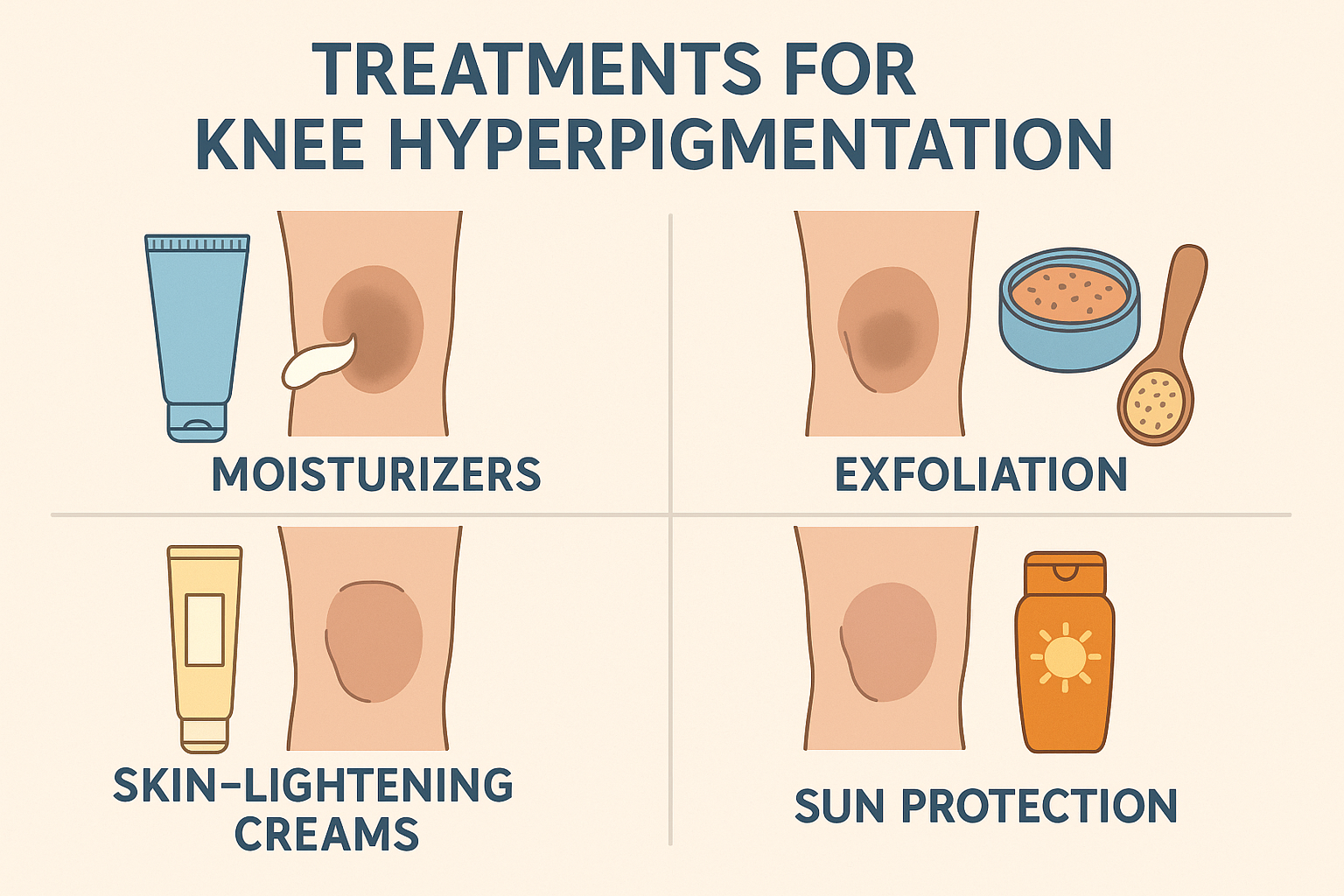
Combining Nizoral with the right skincare products can boost your results—if done smartly. Start with gentle exfoliants like salicylic acid to prep the skin and reduce oil buildup. While it’s not antifungal, it helps create a less favorable environment for yeast.
Niacinamide is another excellent match. It soothes the skin, strengthens the skin barrier, and helps regulate sebum production—without clogging pores.
But steer clear of heavy oils like coconut or olive oil. These can feed Malassezia and make fungal acne worse. Also, avoid overly occlusive products that trap moisture and heat on the skin.
Keep your routine simple: gentle cleanser, Nizoral, and lightweight moisturizers. Let your skin breathe and recover. If you’re unsure which combinations are safe, ask your dermatologist for personalized guidance.
Final Thoughts
Fungal acne is often mistaken for regular acne—and that’s why many treatments fail. Unlike bacterial breakouts, fungal acne needs a different approach. Understanding the root cause is the first step toward effective care.
If you live in a humid area, sweat often, or use antibiotics regularly, you could be at higher risk. In these cases, traditional cleansers may not work, and antifungal products like Nizoral can deliver better, faster results.
But skincare isn’t just about one product. Combining Nizoral with ingredients like salicylic acid and niacinamide helps improve skin texture and prevent future breakouts—while avoiding pore-clogging oils is just as important.
Know your skin, choose your products wisely, and stay consistent. With the right approach, fungal acne can be treated and prevented for the long term.






 Acne
Acne Anti-Aging
Anti-Aging Business
Business Digital Marketing
Digital Marketing Economics
Economics Exfoliation
Exfoliation Hair Removal
Hair Removal Movies
Movies Personal Finance
Personal Finance Websites
Websites