Nodular Acne Treatment: Dermatologists’ Top Advice
Clear, healthy skin doesn’t always come easy—especially when you’re dealing with nodular acne. Unlike surface-level pimples, this severe form of acne forms deep within the skin, often causing pain and inflammation without any visible “head.” Dermatologists describe it as the “iceberg” of acne—what you see is just a small part of what’s underneath.
Because it doesn’t respond well to over-the-counter products, nodular acne requires professional care. If ignored, it can lead to long-lasting scars and damage to skin structure.
This article breaks down the expert-approved ways to recognize, understand, and treat nodular acne. Whether you’re just starting your skincare journey or have been battling stubborn breakouts, this guide offers science-backed solutions that can actually make a difference.
What Does Nodular Acne Look Like?
Nodular acne appears as hard, painful lumps beneath the skin, with no visible whitehead or blackhead. These nodules are deeply embedded in the dermis—the layer filled with nerves and collagen—which explains the intense discomfort.
Unlike mild acne, these breakouts feel firm and can be flesh-toned or reddish due to inflammation. They don’t come to a head and can’t be popped, making self-treatment risky and often ineffective.
Left untreated, nodular acne can destroy collagen and leave behind deep scars. That’s why early diagnosis and treatment by a dermatologist are crucial. Recognizing the signs early increases the chance of preventing permanent skin damage and getting clearer, healthier skin faster.
What Triggers Nodular Acne?
Nodular acne is usually caused by a combination of internal and external factors. Genetics play a big role—if severe acne runs in your family, you’re more likely to develop it too. Hormonal changes, especially increased androgen levels, can also trigger oil production, clogging pores and feeding inflammation.
Other common causes include:
- Excess oil (sebum) production
- Dead skin cell buildup blocking pores
- Cutibacterium acnes, a skin bacteria that worsens deep breakouts
Certain medications, like steroids or lithium, which may disrupt skin balance
Since the causes vary from person to person, treatment is rarely one-size-fits-all. Dermatologists often recommend a tailored approach that addresses both surface-level symptoms and internal imbalances.
Nodular Acne vs. Cystic Acne: What’s the Difference?
Though often confused, nodular and cystic acne are not the same. Both types form deep under the skin and are painful, but their texture and appearance differ.
Cystic acne contains pus, making it softer and often redder. It usually forms large, inflamed bumps that may eventually ooze. Nodular acne, on the other hand, feels hard and solid, like a knot beneath the skin. It doesn’t have pus and may not appear as inflamed on the surface.
Both are serious and should never be popped. Doing so can lead to deeper infections and permanent scarring. The safest route? A dermatologist-guided treatment plan to prevent long-term skin damage and speed up recovery.
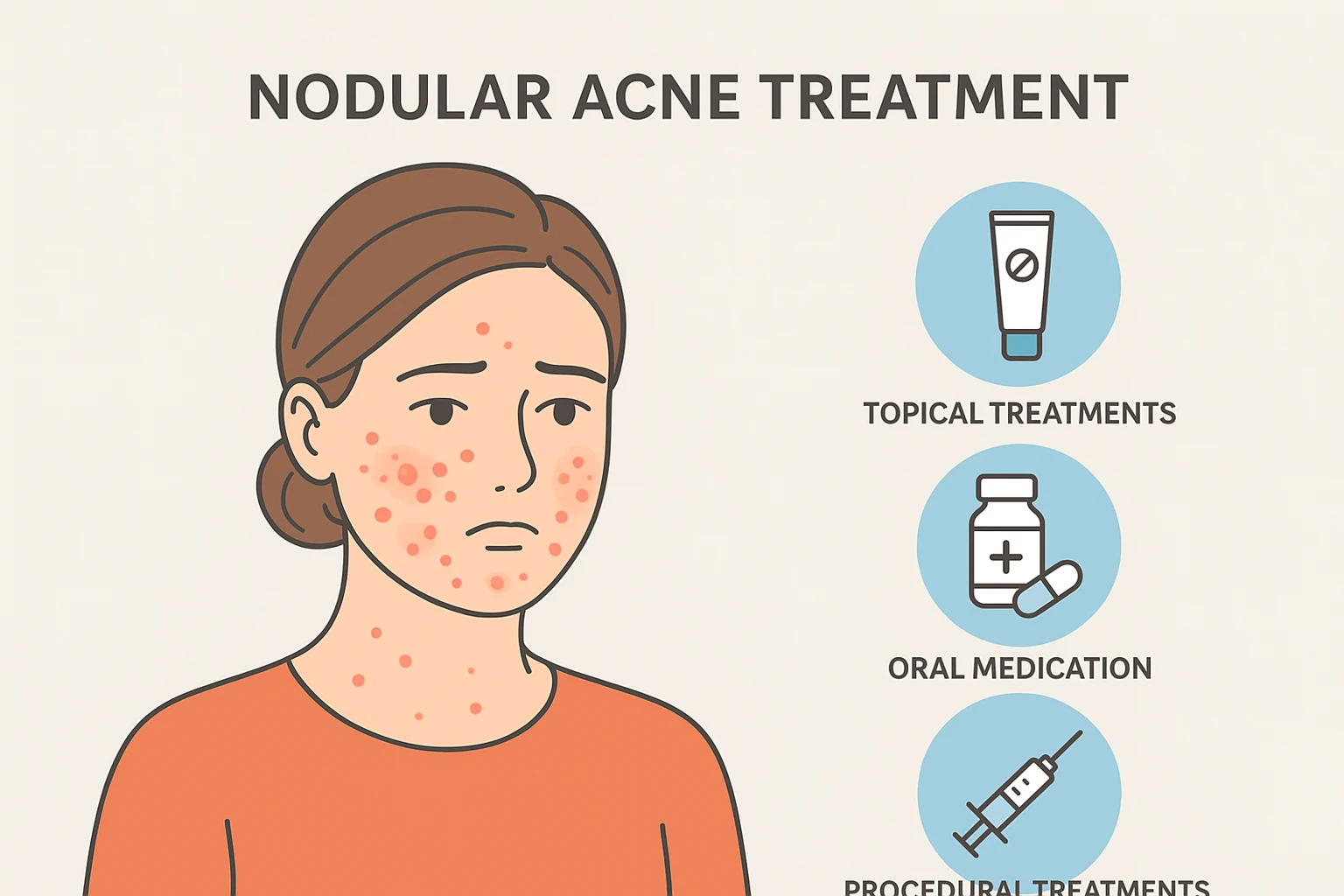
How to Treat Nodular Acne Effectively
Topical creams aren’t enough for nodular acne because they can’t reach the deep layers of the skin where these breakouts form. According to dermatologists, systemic treatments—such as oral antibiotics, hormonal therapy, or isotretinoin—are often needed.
Oral medications help reduce internal inflammation, regulate oil production, and prevent bacterial overgrowth from within. For women, hormonal birth control can help balance hormone-related breakouts.
The key is early treatment. Don’t wait for the nodule to shrink on its own—it likely won’t. The sooner you see a board-certified dermatologist, the better your chances of avoiding permanent scars and getting smoother skin.
Oral Medications
Because nodular acne forms deep in the skin, oral medications are often essential for successful treatment. Dermatologists typically recommend the following options:
- Spironolactone
Commonly prescribed for women, this medication blocks androgen hormones like testosterone, reducing oil production and preventing clogged pores. - Oral contraceptives (birth control pills)
By regulating hormone levels, certain birth control pills help control hormonal acne flare-ups, especially on the jawline and chin. - Oral antibiotics
These target inflammation and reduce the growth of Cutibacterium acnes, the bacteria commonly involved in deep acne. - Isotretinoin (Accutane)
A powerful vitamin A derivative, isotretinoin shrinks oil glands and can permanently reduce sebum production. It’s highly effective but must be taken under strict medical supervision due to potential side effects. - Topicals and retinoids
Though not enough on their own, topical treatments like retinol complement oral medications by improving skin texture, preventing new breakouts, and fading dark spots or acne scars.
Using a combination of oral and topical treatments offers the best results—especially when managed by a board-certified dermatologist.
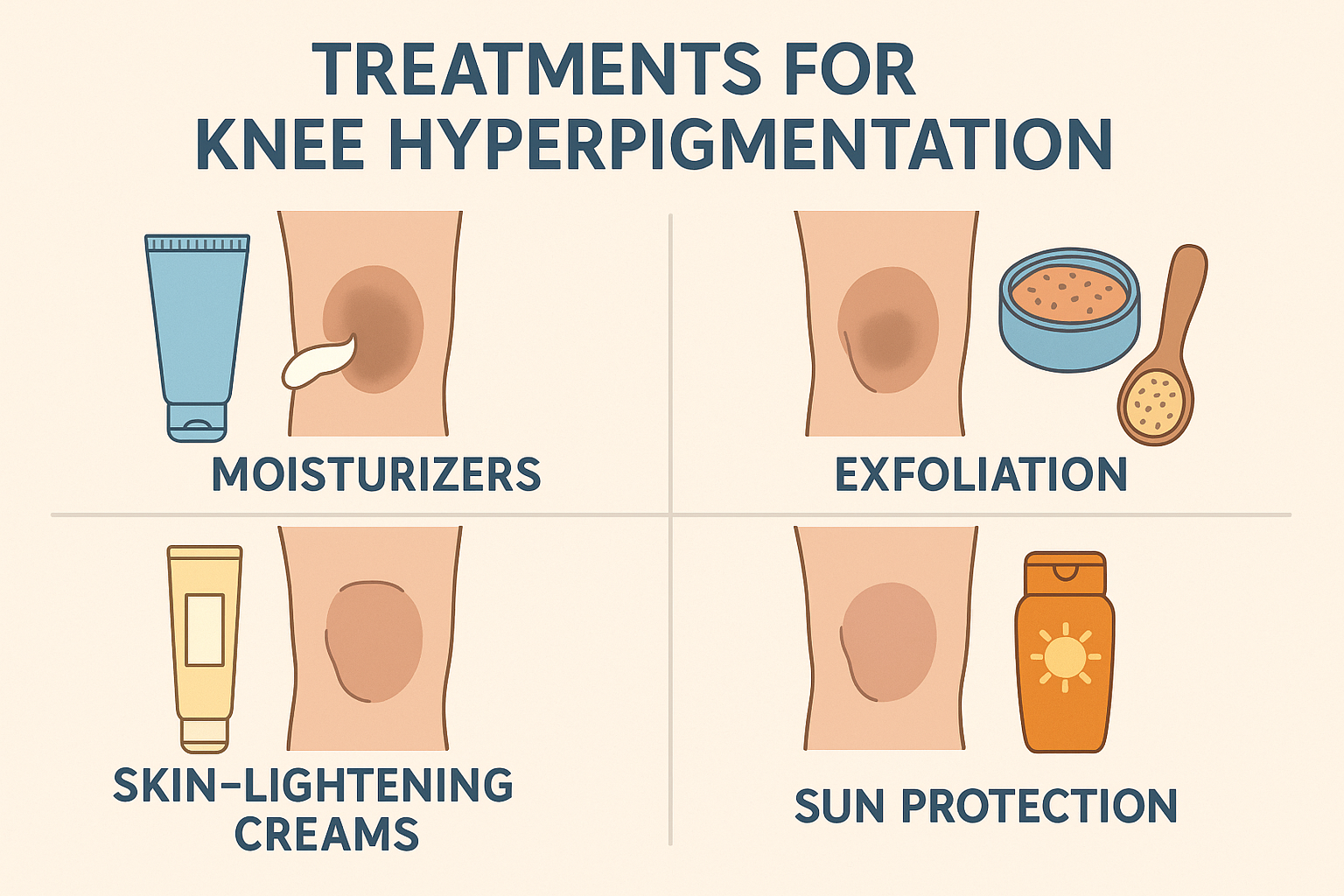
Topical Treatments
Although nodular acne develops deep beneath the skin, topical treatments still play a valuable support role in your routine. They help control surface oil, reduce bacteria, and prevent new clogged pores.
Two of the most effective topical ingredients include:
- Salicylic acid
This chemical exfoliant unclogs pores by removing dead skin cells and reducing inflammation. It helps keep the skin clear and less prone to new breakouts. - Benzoyl peroxide
Known for its antibacterial properties, this ingredient kills C. acnes bacteria and helps reduce redness and swelling. It also controls excess oil production on the skin’s surface.
While topical treatments alone can’t cure nodular acne, they enhance the effectiveness of oral medications. Dermatologists often recommend combining both approaches for a faster and more lasting improvement in skin health.
In-Clinic Treatments
When nodular acne is severe or resistant to medications, in-office treatments offer additional relief. These procedures are performed by dermatologists and help reduce inflammation, speed up healing, and minimize scarring.
Popular options include:
- Chemical peels
These treatments use acids to remove dead skin and unclog pores. They also stimulate collagen production and improve skin texture over time. - Corticosteroid injections
Steroids are injected directly into large, painful nodules to reduce swelling and pain quickly. This method works well for isolated breakouts. - Minor incisions
In rare cases, a dermatologist may perform a small incision to release trapped pus and debris inside a nodule. This must be done in a sterile clinical setting to avoid further infection or scarring.
In-office treatments can be powerful allies in your acne recovery plan, especially when combined with a personalized skincare and medication routine.
How to Spot Nodular Acne
Identifying nodular acne early is essential to prevent scarring and worsening symptoms. Unlike typical pimples, nodular acne is rooted deep within the skin and feels like a firm, painful lump.
These breakouts are usually:
- Hard to the touch
- Painful even without pressure
- Red or skin-colored
- Lacking a visible whitehead or pus
Common areas include the chin, jawline, neck, and back—places rich in oil glands. According to Dr. Rachel Nazarian, a board-certified dermatologist, “Nodules should never be popped. They need medical intervention to avoid deep scarring.”
If you notice these signs, don’t wait. Early treatment from a dermatologist can significantly improve your skin outcome.
Where Does Nodular Acne Commonly Appear?
Nodular acne can show up almost anywhere, but certain areas are more prone due to higher oil production and friction. Knowing where it usually appears helps you take preventive steps early.
- Face (especially jawline and chin)
Hormonal fluctuations make this area a hot spot—especially in women experiencing adult acne. - Back (a.k.a. bacne)
Friction from backpacks, tight clothing, and sweat can trigger deep breakouts along the spine and shoulders. - Chest
Sweat and oil can accumulate here, especially during workouts or hot weather. - Neck and shoulders
Frequently exposed to sweat, hair products, or collars—these areas are common zones for stubborn breakouts.
Maintaining hygiene, avoiding pore-clogging products, and choosing breathable fabrics are smart ways to reduce nodular flare-ups. If breakouts persist in these areas, it’s a good idea to speak with a dermatologist.
How to Prevent Nodular Acne from Coming Back
Preventing nodular acne isn’t just about having clean skin—it’s about building a smart, consistent routine and understanding your triggers. Since this type of acne tends to be chronic, long-term prevention is essential.
Here are dermatologist-approved tips to keep flare-ups at bay:
- Choose non-comedogenic products
Opt for moisturizers, sunscreens, and makeup labeled as “non-comedogenic” to avoid clogging pores. - Exfoliate gently
Use mild exfoliants like salicylic acid once or twice a week to clear out dead skin cells and prevent buildup—without irritating your skin. - Watch your diet and sleep habits
Sugary foods and poor sleep can disrupt hormones and trigger breakouts. Aim for balanced meals and consistent rest. - Manage your stress
Chronic stress increases cortisol, which stimulates oil production and may worsen acne.
Even when your skin starts to clear, continue using prescribed topical or oral treatments. According to Dr. Marisa Garshick, a board-certified dermatologist, “Maintenance is just as important as the initial treatment when it comes to preventing recurrence.”
Consistency is key. With the right habits and follow-through, you can help keep your skin clearer and more resilient over time.






 Acne
Acne Anti-Aging
Anti-Aging Business
Business Digital Marketing
Digital Marketing Economics
Economics Exfoliation
Exfoliation Hair Removal
Hair Removal Movies
Movies Personal Finance
Personal Finance Websites
Websites