11 Reasons Your Acne Won’t Go Away, According to Derms

Still breaking out despite trying every product you can find? Persistent acne can be incredibly frustrating, especially when nothing seems to work. But here’s the truth: acne is rarely caused by just one thing. Instead, it’s usually triggered by a combination of factors—hormones, stress, diet, and even how your skin reacts to skincare products.
According to dermatologists, hormonal acne often appears on the cheeks and jawline, especially around your period. Meanwhile, forehead breakouts might be linked to excess oil, diet, or sweat buildup.
Dr. Marissa Garshick, board-certified dermatologist, says recognizing where and when your acne shows up can help pinpoint the root cause. “If acne isn’t improving, it’s often a sign of an overlooked trigger,” she explains.
Keep reading to discover 11 common—and sometimes surprising—reasons your acne won’t go away. You’ll also learn practical tips on how to manage each one effectively, whether you’re new to skincare or just trying to level up your routine.
11 Possible Reasons Acne Won’t Go Away
1. You’re Dealing with Hormonal Acne
Hormonal acne isn’t just for teenagers—it’s also common in adults, especially women in their 20s and 30s.[1Skroza N, Tolino E, Mambrin A, et al. Adult acne versus adolescent acne: a retrospective study of 1,167 patients. J Clin Aesthet Dermatol. 2018;11(1):21-25.] These breakouts often appear on the lower face, like the jawline or chin, and tend to flare up around your period, during pregnancy, or due to hormonal imbalances like PCOS.
During hormonal shifts, oil glands can go into overdrive, clogging pores and triggering inflammation. “Hormonal acne tends to be deeper and more painful,” says Dr. Shereene Idriss, a board-certified dermatologist.
Treating it effectively often means balancing hormones from the inside out. Some options include birth control pills, spironolactone (an anti-androgen medication), or skincare with ingredients like salicylic acid and retinoids. Keep in mind that consistency is key—results won’t appear overnight.
Understanding your hormone patterns and adjusting your skincare accordingly can be the game-changer you need.
2. Your Skincare Products Don’t Match Your Skin Type
Not all skincare is created equal—and using the wrong products for your skin type can actually make acne worse. Oily skin needs different care than dry or sensitive skin, and harsh products can strip your skin’s natural barrier, leading to more breakouts.
Ingredients like benzoyl peroxide are effective against acne-causing bacteria and excess oil. Salicylic acid helps unclog pores and reduce inflammation. However, overuse or layering too many actives can backfire, especially on acne-prone skin.[2Kawashima M, Nagare T, Doi M. Clinical efficacy and safety of benzoyl peroxide for acne vulgaris: comparison between Japanese and Western patients. J Dermatol. 2017;44(11):1212-1218. doi:10.1111/1346-8138.13996.]
According to Dr. Whitney Bowe, a leading dermatologist, “Start simple and build up. Choose one active ingredient and give it time before adding more.”
Also, look for labels that say “non-comedogenic” or “oil-free” to avoid pore-clogging formulas. Customizing your skincare to your actual skin needs—not trends—can make a huge difference in clearing acne.
3. You Only Treat Active Breakouts
One major mistake many beginners make is spot-treating pimples instead of treating the whole face. But acne starts forming under the skin weeks before it shows up, meaning prevention is just as important as treatment.
Dr. Sandra Lee (aka Dr. Pimple Popper) emphasizes the need for full-face treatment: “If you only treat visible pimples, you’re always playing catch-up.”
Using products like retinoids or salicylic acid consistently over the entire face helps prevent clogged pores and stops breakouts before they start. Focus especially on acne-prone areas like the T-zone and jawline.
Preventive care builds long-term results. Think of it as training your skin to stay clear—not just putting out fires when pimples pop up.
4. You’re Treating the Wrong Type of Acne
Not all acne is created equal—and treating the wrong type can make things worse. Knowing whether your breakouts are hormonal, bacterial, or fungal is key to finding the right solution.
Hormonal acne often appears along the jawline, chin, and neck, flaring up during periods, pregnancy, or hormonal shifts. Meanwhile, bacterial acne is more common for oily skin types and can be triggered by clogged pores, sweat, or environmental dirt.
Then there’s fungal acne—a lesser-known but common issue caused by yeast overgrowth. Unlike typical acne, it doesn’t respond to standard treatments. According to dermatologists, antifungal products like ketoconazole shampoo (e.g., Nizoral) are more effective here.
If your skincare isn’t working, it might be because you’re targeting the wrong problem. Identifying your acne type accurately will help you choose products that actually work—and clear your skin faster.
5. You’re Overusing Skincare Products
When it comes to acne, more is not always better. Overloading your skin with multiple active ingredients can lead to irritation, dryness, and even more breakouts.
Common mistake? Layering salicylic acid cleanser with a toner and spot treatment that also contain harsh actives like benzoyl peroxide or retinoids. This cocktail can strip your skin barrier, causing redness and sensitivity.
Dr. Rachel Nazarian, board-certified dermatologist, advises: “Stick to one or two targeted actives, and use them consistently instead of throwing everything at once.”
If your skin feels tight, flaky, or burns after applying products, it’s a sign you’re overdoing it. Simplify your routine and give your skin time to adjust—it’ll reward you with better results.
6. You’re Not Consistent with Your Routine
Even the best skincare won’t work if you’re not using it regularly. Skipping essential steps—like cleansing at night—can clog pores and undo progress.
Inconsistency, even just a few missed nights, can slow down healing and trigger new breakouts. Dermatologists agree: routine is everything. Cleansing, treating, moisturizing, and protecting your skin with SPF should be part of your daily habits—not just during flare-ups.
Feel overwhelmed? Keep it simple. A beginner-friendly acne routine includes:
- Cleanser (twice a day)
- Acne treatment (once daily or as prescribed)
- Lightweight, non-comedogenic moisturizer
- Broad-spectrum sunscreen in the morning
- Small, consistent steps lead to big improvements over time.
7. Your Lifestyle Habits Are Making Acne Worse
Your skincare might be on point—but daily habits could be sabotaging your skin. Many people overlook how environment and hygiene affect breakouts.
Here are lifestyle triggers to watch out for:
- Dirty pillowcases or towels—these collect oil and bacteria, transferring them to your skin.
- Sharing makeup tools—spreads acne-causing bacteria.
- Infrequent hair washing—oil from your hair can clog forehead pores.
- Leaving makeup on overnight—traps bacteria and irritants in your pores.
- Not cleansing after sweating—sweat can mix with oil and block pores if left on the skin.
A few small changes—like washing pillowcases weekly and keeping your hands off your face—can drastically improve your skin health.
8. Your Diet Isn’t Skin-Friendly
What you eat shows up on your skin. While food alone doesn’t cause acne, some choices can trigger inflammation or hormonal shifts that worsen it.
High-glycemic foods (think sugary snacks or white bread) can spike insulin levels, which in turn raises androgen hormones—leading to excess oil and breakouts. Dairy, particularly cow’s milk, is also linked to acne in some individuals due to natural hormones it contains.[3American Academy or Dermatology Association. Can the right diet get rid of acne?]
On the flip side, a diet rich in antioxidants—like berries, leafy greens, and omega-3s—helps reduce inflammation and support skin repair. According to Dr. Mona Gohara, Associate Clinical Professor of Dermatology at Yale, “A balanced diet is a powerful tool in long-term acne care.”
Pair smart eating with consistent skincare for a clearer, healthier complexion from the inside out.
9. You Keep Popping Pimples
Popping pimples might feel satisfying—but it’s one of the worst things you can do for your skin. Squeezing a zit forces bacteria, oil, and debris deeper into your pores, increasing inflammation and the risk of scarring.
Dr. Muneeb Shah, dermatologist and content creator, warns that “picking at acne often leads to post-inflammatory hyperpigmentation and permanent damage.”
Even worse, touching inflamed pimples like cysts or nodules can spread bacteria, causing breakouts to multiply. If you have painful, deep acne, resist the urge to pick and let a dermatologist handle professional extraction or corticosteroid injections instead.[4Pimple popping: Why only a dermatologist should do it. (n.d.). Retrieved January 26, 2022.]
Avoiding this habit not only prevents scarring but also helps your skin heal faster and more evenly.
10. You May Have an Underlying Medical Condition
When acne refuses to go away, even after months of skincare, it might be linked to an underlying medical issue. Hormonal imbalances—especially from endocrine disorders—are a common but overlooked cause.
Polycystic Ovary Syndrome (PCOS), for instance, leads to elevated androgen levels, which trigger oil overproduction and persistent acne along the jawline. Other rare conditions like Cushing’s syndrome or acromegaly may also affect hormone levels and skin health.
There are even non-hormonal syndromes like PAPA or SAPHO that can manifest as chronic acne.
If your breakouts are unusual, painful, or resistant to typical treatments, see a doctor. A thorough medical evaluation could uncover a root cause—and help you get clearer skin from the inside out.
11. It’s Time to See a Dermatologist
Tried every OTC product with no luck? If your acne hasn’t improved in two to four weeks, it’s time to consult a dermatologist.
For moderate to severe breakouts, prescription treatments like Epiduo Forte Gel (which combines adapalene and benzoyl peroxide) can significantly reduce inflammation and unclog pores. According to Dr. Dendy Engelman, this combo is one of the most effective for stubborn acne.
Severe cases may also require oral antibiotics or hormone-regulating medications like spironolactone. For cystic acne, isotretinoin—commonly known by its brand name Accutane—is often recommended under close supervision.
A board-certified dermatologist will customize a treatment plan based on your skin type, acne severity, and medical history—ensuring safer and faster results.
How to Tell If It’s Acne or Something Else
Not every bump on your face is acne. Knowing the difference helps you avoid the wrong treatment and unnecessary irritation.
Acne typically includes blackheads, whiteheads, papules (small red bumps), or pustules (pimples with pus), often appearing in oily zones like the forehead, nose, and chin. These are caused by clogged pores and overactive oil glands.
But other skin conditions can mimic acne:
- Rosacea: Chronic redness and small bumps, usually mistaken for adult acne.
- Folliculitis: Inflamed hair follicles, sometimes due to bacteria or yeast.
- Milia: Tiny white cysts, not related to oil or clogged pores.
- Perioral Dermatitis: Acne-like rash around the mouth, often triggered by steroid creams or toothpaste.
If your “acne” isn’t responding to products like benzoyl peroxide or salicylic acid within a few weeks, get a professional diagnosis. The right ID leads to the right solution.
The Link Between Stress, Mental Health, and Acne
Stress doesn’t just affect your mood—it shows up on your skin too. When you’re stressed, your body produces more cortisol, a hormone that boosts oil production and worsens breakouts.
Dr. Alexis Stephens, board-certified dermatologist, explains that “stress-related acne is often overlooked but can trigger flare-ups and delay healing.”
Stress can also disrupt sleep and lead to unhealthy habits like skipping skincare or eating sugary comfort food—both of which can make acne worse. Plus, chronic anxiety and depression may increase inflammation in the body, making acne more persistent and painful.
Managing stress is just as important as using the right products. Try adding stress-reducing habits like yoga, journaling, or even therapy to your routine. Clear skin often starts with a calm mind.
Common Skincare Mistakes That Make Acne Worse
Trying too hard to fight acne? You might be making it worse without realizing it. Dermatologists say that simple skincare mistakes can damage your skin barrier and trigger even more breakouts.
Over-washing your face—more than twice a day—can strip away natural oils, causing your skin to produce more sebum as a rebound effect. This leads to clogged pores and inflammation.
Other common mistakes include:
- Using harsh products, like alcohol-based toners or abrasive scrubs, which irritate the skin.
- Layering too many actives at once—such as retinol, AHA, and BHA—can overwhelm and inflame your skin.
- Not removing makeup properly, which traps dirt and oil inside pores.
- Popping pimples, which spreads bacteria and increases the risk of scarring.
The best approach? Keep it simple. Experts recommend using a gentle cleanser, non-comedogenic moisturizer, and one or two actives that suit your skin. In acne care, less really is more—and consistency always wins.
Recommended Skincare Routine for Acne-Prone Skin (AM & PM)
A clear-skin routine doesn’t have to be complicated—just smart and consistent. For acne-prone skin, dermatologists suggest a focused morning and evening routine that reduces oil, unclogs pores, and prevents irritation.
Morning Routine:
- Gentle cleanser – Use a mild face wash (e.g., CeraVe Foaming Cleanser) to remove excess oil.
- Toner (optional) – Choose an alcohol-free, soothing formula.
- Lightweight serum – Try niacinamide to balance oil and calm redness.
- Oil-free moisturizer – A gel texture works well for acne-prone skin.
- Broad-spectrum SPF 30+ – Essential to prevent sun-triggered inflammation.
Night Routine:
- Double cleansing – Start with micellar water, followed by a gentle face wash.
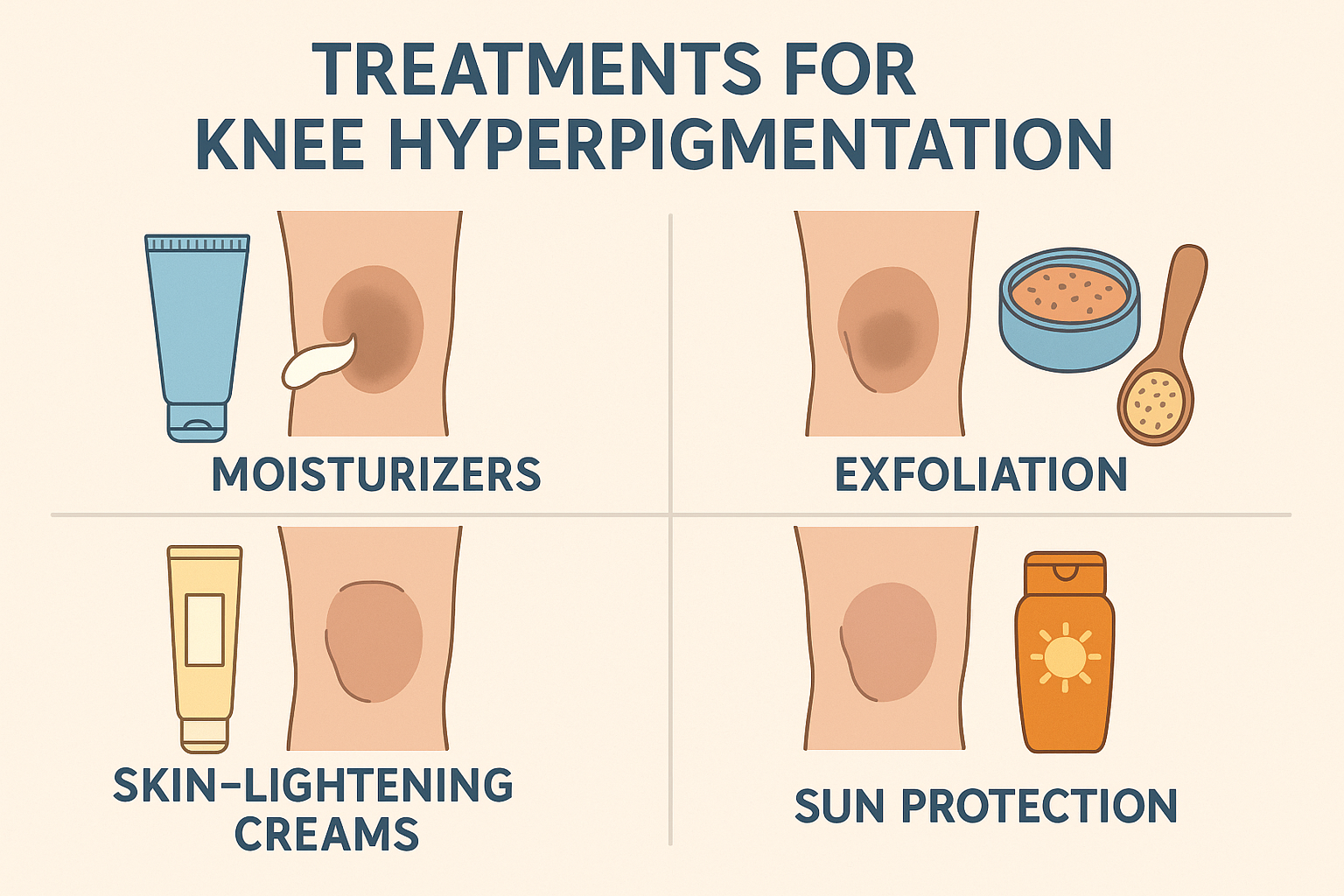
- Mild exfoliation (2–3x/week) – Use BHA or salicylic acid to clear pores.
- Spot treatment (if needed) – Benzoyl peroxide or sulfur-based creams work well.
- Night moisturizer – Helps skin recover overnight.
Stick with your routine and don’t rush results. According to dermatologists, a simple, balanced regimen done consistently will outperform complex routines that stress the skin.






 Acne
Acne Anti-Aging
Anti-Aging Business
Business Digital Marketing
Digital Marketing Economics
Economics Exfoliation
Exfoliation Hair Removal
Hair Removal Movies
Movies Personal Finance
Personal Finance Websites
Websites